Academic Support for Nursing Students
No notifications.
Tagged as: diagnosis

Chapter 3: Measuring and Recording the Vital Signs
Introduction.
The measurement and recording of the vital signs is the first step in the process of physically examining a patient - that is, in collecting objective data about a patient's signs (i.e. what the nurse can observe, feel, hear or measure). This is a fundamental skill for nurses working in all clinical areas, but one which only develops with practice. This chapter introduces the knowledge and skills required by nurses to accurately measure and record a patient's vital signs - that is, their blood pressure (BP), pulse or heart rate (HR), temperature (T°), respiratory rate (RR) and blood oxygen saturation (SpO 2 ).
This chapter begins with an introduction to the importance of measuring the vital signs in nursing practice. It goes on to describe the measurement of each of the vital signs and the collection of other supporting data (e.g. height, weight, pain score), discussing key strategies and considerations. The chapter then reviews the processes involved in recording the data collected about the vital signs. Finally, the chapter discusses how a nurse should go about interpreting the data they have obtained, to build a clinical picture of the patient and plan for their care.
Learning objectives for this chapter
By the end of this chapter, we would like you:
- To describe the place of measuring and recording the vital signs in the health observation and assessment process.
- To state the normal parameters of each vital sign for a healthy adult.
- To understand how to accurately measure each vital sign.
- To understand how to collect other key health data (e.g. height, weight, pain score).
- To describe how to correctly record this data.
- To explain how this data should be interpreted and used in nursing practice.
Important note
This section of the chapter assumes a basic knowledge of human anatomy and physiology. If you feel you need to revise these concepts, you are encouraged to consult a quality nursing textbook.
If you need assistance with writing your essay, our professional nursing essay writing service is here to help!
Measurement and recording of the vital signs
As described in the introduction of this chapter, the measurement and recording of the vital signs is a fundamental skill for nurses working in all clinical areas. The vital signs - blood pressure (BP), pulse or heart rate (HR), temperature (T°), respiratory rate (RR) and blood oxygen saturation (SpO 2 ) - provide baseline indicators of a patient's current health status. It is important to note that some nurses measure and record the vital signs at the commencement of the physical examination, while others integrate the collection of vital signs data into the physical examination; either approach is fine, provided the nurse is systematic in the way in which they approach their assessment, and so collects accurate and complete health data.
As you saw in the previous chapter of this module, health observation and assessment involves three concurrent steps:

The measurement and recording of the vital signs is the first step in the process of physically examining a patient. This step involves collecting objective data - that is, data about a patient's signs (i.e. what the nurse can observe, feel, hear or measure). Data collected during the physical examination, including measurements of the vital signs, is combined with that collected during the health history (as described in the previous chapter of this module), to build a complete picture of the clients' health status.
The normal parameters for each of the vital signs of healthy adults are listed following:
|
|
|
| Blood pressure (BP) | 120/80 mmHg |
| Pulse or heart rate (HR) | 60-100 beats per minute |
| Temperature (T°) | 36.5°C to 37.5° Celsius |
| Respiratory rate (RR) | 10 to 16 breaths per minute |
| Blood oxygen saturation (SpO ) | 98%-100% |
Nurses should become thoroughly familiar with the parameters for each of the vital signs. However, it is important for nurses to remember that these are average values for healthy adults. Some adults may have values which fall outside of these ranges. For example, very fit adults may have a pulse or heart rate which normally sits at or below 60 beats per minute; similarly, adults with respiratory conditions often have an oxygen saturation which normally sits well below 98%. Children and neonates have differing normal parameters for each of the vital signs; nurses who work with these patient groups must become familiar with these. When interpreting vital signs, it is important that nurses use critical thinking to interpret the entire clinical picture of the individual patient with whom they are working.
Measurement of blood pressure
Blood pressure is often abbreviated to 'BP'. Blood pressure uses two measurements, each recorded in millimetres of mercury (mmHg) - for example, 120mmHg / 80mmHg, often abbreviated to 120/80. Blood pressure is defined as the pressure of the blood against the arterial walls:
- When the heart contracts (systolic BP - the first measurement), and
- When the heart rests (diastolic BP - the second measurement).
Essentially, blood pressure is a measurement of the relationship between: (1) cardiac output (the volume of blood ejected from the heart each minute), and (2) peripheral resistance (the force that opposes the flow of blood through the vessels). Blood pressure also depends on factors such as the velocity of the blood, the intravascular blood volume and the elasticity of the vessel walls, etc.
The difference between the systolic and diastolic blood pressures is referred to as the pulse pressure . This normally ranges between 30mmHg and 40mmHg.
Blood pressure can be measured in a number of different ways. It is measured directly by inserting a small catheter into an artery - however, as a very invasive procedure, this strategy is typically only used for patients who are critically ill and for whom blood pressure is very difficult to measure accurately. In all other settings, blood pressure is measured indirectly using: (1) a sphygmomanometer and a stethoscope (a 'manual' measurement), or (2) a non-invasive blood pressure monitor (an 'automatic' measurement). This section of the chapter will teach both methods.
| It is important that nurses familiarise themselves with the equipment used to measure the vital signs. Review the image of a sphygmomanometer to the left, which is labelled with the device's key features:
|
|
- Measuring blood pressure using a sphygmomanometer and a stethoscope (a 'manual' measurement): The client should be sitting or lying down. The arm used to take the blood pressure should be at the client's side, slightly flexed and with the palm turned upwards. The nurse should palpate the brachial pulse, in the antecubital space (i.e. the groove between the biceps and triceps muscles, in the bend of the elbow). A blood pressure cuff should be placed 2.5 centimetres above the site of the brachial pulse, with the bladder of the cuff (usually marked with a white stripe) centred over the artery. The cuff should be secured so it fits evenly and snugly around the arm.
The manometer - the device used to read the blood pressure measurement - should be positioned at the nurse's eye level. The valve on the pressure bulb should be closed by turning it clockwise. Avoid closing the valve too tightly, or it may be too difficult to release when the time comes to do so.
Place the stethoscope over the patient's brachial pulse, and hold it with your non-dominant hand. Place the binaurals (earpieces) of the stethoscope in your ears. Using your dominant hand, inflate the cuff to around 180mmhg (note that you may need to go higher if the patient's systolic blood pressure is >180mmHg, however this is rare). Then, release the valve to deflate the cuff, slowly and steadily (around 2 to 3mmHg per second to reduce measurement errors). You are listening for two things:
- The first Korotkoff sound. This is a sharp thump or tap of the brachial pulse, which indicates the systolic blood pressure. Read the pressure (in mmHg) on the manometer at the point this occurs.
- The disappearance of all Korotkoff sounds (i.e. all the noises related to the brachial pulse). This indicates the diastolic blood pressure. Read the pressure (in mmHg) on the manometer at the point this occurs.
Once these two measurements have been made, the cuff should be completely deflated and removed from the client's arm. The two blood pressure readings should be promptly recorded.
- Measuring blood pressure using a non-invasive blood pressure monitor (an 'automatic' measurement): This is achieved using the same principles as with the manual measurement, described above. However, it involves using an electronic monitoring device; this measures the circulating blood flow using an electronic sensor and, therefore, does not require the nurse to listen for Korotkoff sounds. The cuff of an automatic blood pressure monitor is applied in the same way as described above. The nurse then presses a 'start' button to instruct the machine to inflate the cuff, take a measurement and provide a reading.
It is important to highlight that although automatic blood pressure measurements are quick and convenient, they are not as accurate as manual blood pressure measurements. If a non-invasive blood pressure monitor returns a reading which is outside the expected parameters, it should always be checked with a manual measurement. Furthermore, it is worth noting that a cuff must fit correctly on a patient's arm, and be placed correctly so the bladder of the cuff is above the brachial artery, if a non-invasive blood pressure monitor is to return an accurate reading.
As described in the above section, the upper arm is the most common site to measure blood pressure; however, if this is not possible, blood pressure may also be measured from the thigh. Research suggests that the systolic blood pressure is slightly higher in the leg than in the arm, but the diastolic blood pressures are roughly similar. Blood pressure is taken on the thigh using the same technique described above.
In some cases, a patient may have their blood pressure taken a number of times in a number of positions (e.g. lying, sitting, standing). This is done to assess the client for orthostatic hypotension . This occurs when there is a 20 to 30mmHg drop in blood pressure when the client changes positions, and it may indicate health problems.
It is important for nurses to note that there are a number of common errors associated with blood pressure measurement. Errors may result if:
- The client's arm is positioned above or below the level of their heart.
- The cuff used is too large or too narrow for the client's arm.
- The cuff is wrapped too loosely or unevenly around the client's arm.
- The cuff is not deflated to a pressure higher than the patient's systolic blood pressure.
- The cuff is deflated at a rate slower or faster than 2 to 3mmHg per second.
- The cuff is reinflated (e.g. to check readings) before it is completely deflated.
- The stethoscope is pressed too firmly against the brachial artery.
- The nurse fails to wait 2 minutes before repeating the blood pressure measurement.
As described above, the majority of the common errors associated with blood pressure measurement are related to the size and position of the cuff. Blood pressure cuffs come in a variety of sizes, and it is essential that nurses select the correct size for the individual patient with whom they are working - if the cuff is too large, blood pressure will be underestimated, and if it is too small, blood pressure will be overestimated. Ideally, the width of the cuff should be 40% of the circumference of the limb from which the blood pressure is being measured, and the bladder within must encircle at least 80% of the limb.
As you saw in an earlier section of this chapter, the average blood pressure of a healthy adult is 120mmHg/80mmHg, typically written as 120/80. When measuring a client's blood pressure, a nurse may identify that it is high - a condition referred to as hypertension , or low - a condition referred to as hypotension . There may be a number of pathophysiological causes of hypertension (e.g. brain injury, systemic vasoconstriction, fluid retention, etc.) and hypotension (e.g. fluid / blood loss, dehydration, etc.). It is important for nurses to recognise that there are also a number of physiological factors which affect blood pressure measurement; for example, recent exercise, feeling anxious or angry, experiencing pain, ingesting caffeine or tobacco, and obesity can all result in a patient recording higher than normal blood pressure. Remember: when interpreting vital signs, it is important that nurses use critical thinking to interpret the entire clinical picture of the individual patient with whom they are working.
Measurement of pulse or heart rate
Pulse or heart rate is often abbreviated to 'HR'. It is defined as the number of times a person's heart beats in a one-minute period. It is recorded at a rate of 'beats per minute'. Each contraction of the heart results in the ejection of blood into the vascular system, and this is felt in key locations of the body as a 'pulse'. In addition to assessing the rate at which a person's heart is beating, when measuring a person's HR, a nurse should also assess for the rhythm and quality of the pulse.
A patient's pulse may be measured using the same types of non-invasive, automatic monitors used to measure blood pressure, as described in the previous section of this chapter. However, it is generally preferred that heart rate is assessed by palpating a pulse, and it is this technique which will be taught in this chapter.
To measure a pulse, a nurse should place their fingers over an artery and feel for the pulse. Generally, pulses are palpated with the pads of the index and middle fingers. Firm pressure is applied to the pulse, but not so much pressure that the artery is occluded. There are a number of locations on the body in which a nurse may palpate an artery to feel for a pulse; the most common are:
- The radial artery, located on the outer edge of each wrist.
- The brachial artery, located in the antecubital space on each arm.
- The carotid artery, located on the inner sides of the sternocleidomastoid muscle in the neck.
It is important for nurses to note that a patient's heart rate can also be assessed by auscultating the heart. This is referred to as measuring the apical pulse .
When measuring the HR, a nurse may:
- Count the number of pulses for 60 seconds.
- Count the number of pulses for 30 seconds, and multiply by 2 - if the HR is regular.
- Count the number of pulses for 15 seconds, and multiply by 4 - if the HR is regular.
As described, it is important that a nurse assesses the pulse for regularity. If the pulse is irregular (i.e. the time between each beat varies, or beats are skipped, etc.), the pulse must be counted for one full minute (60 seconds). Additionally, an irregular pulse must be documented when recording the vital signs.
It is also important that the nurse assess the quality of the pulse - that is, its key characteristics. A patient's pulse may be described using terms such as thready (meaning the pulse is 'weak') or bounding (meaning the pulse is 'full' and 'strong'). This is important information that is used, along with HR and regularity of the pulse, to assess the health of the cardiovascular and other body systems.
The average pulse or heart rate for a healthy adult is 60 to 100 beats per minute. If a patient's pulse is >100 beats per minute, this is referred to as tachycardia ; pain, infection, dehydration, stress, anxiety, thyroid disorder, shock, anaemia, certain heart conditions, etc. can all result in tachycardia. If a patient's pulse is <60 beats per minute, this is referred to as bradycardia ; cardiac conduction defects, overdose (e.g. central nervous system depressants), head injury, severe hypoxia (with impending respiratory / cardiac arrest), shock, etc. can all result in bradycardia.
Measurement of temperature
Temperature is often abbreviated to 'T°'. This is defined as the temperature, in degrees Celsius (°C), of a person's body. Temperature is typically measured using a thermometer, which may be either automatic or manual. Temperature may be measured by one of several different routes:
- Orally, with the thermometer placed under the tongue (i.e. in the right or left sublingual pockets). This is the safest way of recording a patient's temperature, and also one of the most accurate. When taking an oral temperature measurement, nurses should take care to ensure the patient has not recently (within the last 10 minutes) ingested hot or cold foods or liquids, that the thermometer is covered by an appropriate shield (for hygiene purposes), and that the patient closes their mouth completely while the thermometer reads their temperature. Automatic thermometers can take up to 30 seconds to record a temperature reading.
- Via the tympanic membrane, with the thermometer placed onto the tympanic membrane within the ear. When taking a tympanic temperature measurement, nurses should take care to ensure that the thermometer is covered by an appropriate shield (for hygiene purposes), and that the sensor comes into contact with all sides of the ear canal.
- Via the axilla, with the thermometer placed under the arm. Although the axilla is a convenient location from which to record a temperature measurement, the accuracy of temperature measurements recorded here are uncertain (i.e. the axilla probably poorly reflects core body temperature).
- Rectally, with the thermometer inserted into the patient's rectum. This is both a safe and accurate way of recording a patient's body temperature, but it is both uncomfortable and invasive; therefore, it is not often used in most clinical settings.
When using an automatic or electronic thermometer to record a patient's temperature, the nurse should place the thermometer in the location on the patient's body at which the temperature is to be recorded, press 'start', and wait for an audible signal and the measurement to register on a display screen. If using a manual thermometer, the thermometer must be located on the patient's body as described, and the nurse must wait at least one full minute before reading the measurement on the gauge of the thermometer. It is worth noting that manual thermometers are rarely used in most clinical settings in the United Kingdom.
The average temperature for a healthy adult is 36.5°C to 37.5°C. If a patient's temperature is >37.5°C, they are said to have hyperthermia or a fever. If a patient's temperature is <36.5°C, they are said to have hypothermia . Causes of variations from normal temperature include infection, stress, dehydration, recent exercise, being in a hot or cold environment, drinking a hot or cold beverage, and thyroid disorders.
Measurement of respiratory rate
Respiratory rate is often abbreviated to 'RR'. This is defined as the number of times a person inhales and exhales in a 1 minute period. It is recorded at a rate of 'breaths per minute'.
Respiratory rate is typically measured by counting the number of times a patient completes a full ventilatory cycle (inhalation plus exhalation) in a 1 minute period. This can be measured by watching the rise and fall of the patient's chest and / or abdomen, or (though less commonly) the breath sounds may also be auscultated. It is best that nurses measure a patient's respiratory rate when the patient is unaware that they are doing so, as this will prevent the patient unconsciously (or even consciously!) changing the way they breathe.
When measuring the RR, a nurse may:
- Count the number of pulses for 30 seconds, and multiply by 2 - if the RR is regular.
- Count the number of pulses for 15 seconds, and multiply by 4 - if the RR is regular.
In addition to assessing a patient's heart rate, the nurse should assess:
- The rhythm, or pattern / regularity, of the patient's breathing.
- The depth of the patient's breathing, or level of lung expansion (normal, shallow, or deep).
- The effort associated with the patient's breathing, often evaluated by observing for accessory muscle use and tissue retractions, etc.
The average respiratory rate for a healthy adult is 10 to 16 breaths per minute. If a patient's RR is >16 breaths per minute, this is referred to as tachpynoea ; this may result from cellular hypoxia, acidosis, conditions that interfere with gas exchange / ventilation / perfusion (e.g. pulmonary oedema, pneumonia, pulmonary embolism), shock, pain, anxiety, asthma, respiratory disease, cardiac disease, etc. If a patient's RR is <10 breaths per minute, this is referred to as bradypnoea ; this may result from head injury, stroke, overdose (particularly of central nervous system depressants), respiratory failure, etc.
Measurement of blood oxygen saturation
Blood oxygen saturation is often abbreviated to 'SpO 2 '. This is defined as the amount of oxygen present in a person's blood - specifically, bound to their haemoglobin - at a given time. It is measured as a percentage, using a non-invasive automatic measuring device called a pulse oximeter. The probe of a pulse oximeter is usually placed on the end of a patient's finger or toe or, less commonly, on their earlobe or their nose. A reading is given on the machine's screen after a period of approximately 15 seconds.
The blood oxygen saturation of a healthy adult is typically 98%-100%. A variety of problems, particularly those related to the respiratory and cardiovascular systems (refer to the information on HR and RR, above), can result in a patient's blood oxygen saturation reducing below this normal range.
Measurement of height, weight and body mass index (BMI)
Although not strictly vital signs, a patient's height, weight and - subsequently - their body mass index (BMI) can provide a nurse with important information about their overall health and physical condition. A patient's weight is measured using a scale, whilst their height is measured using a platform ruler or tape measure. Body mass index can then be calculated, using the following formula: BMI = Weight (kg) / Height (m) 2 It is worth noting that most clinical areas have charts which assist nurses to calculate BMI.
BMI is a useful, objective measurement of a person's body condition, based on their unique height and weight. A patient's BMI is interpreted as follows:
|
|
|
| <18.5 | Underweight |
| 18.6 to 24.9 | Normal weight |
| 25 to 29.9 | Overweight |
| >30 | Obese |
It is worth noting that the accuracy of the BMI measurement - and, therefore, its utility in the clinical context - is subject to much conjecture. As always, it is important that nurses use critical thinking to interpret the entire clinical picture of the individual patient with whom they are working.
Measurement of pain
In many clinical areas, pain is considered the sixth 'vital sign'. Pain is generally assessed using a strategy which can be remembered using the 'OPQRST' mnemonic
| O | Onset: "When did the pain begin?" |
| P | Provocation and palliation: "What makes the pain worse? What helps the pain?" |
| Q | Quality: "Describe the pain." (E.g. sharp, dull, stabbing, etc.). |
| R | Region and radiation: "Where do you feel the pain? Does the pain spread to other areas of your body?" |
| S | Severity: "On a scale of 1 to 10, where 1 is no pain and 10 is the most severe pain you have experienced, how would you rate the pain?" (Note that there are a range of other pain scales - including visual scales for paediatric and non-verbal patients - which may be used in health care settings). |
| T | Time: "How long has the pain been present?" |
It is also important to highlight that there are a number of visual scales which can be used to assess pain in patients who are non-verbal. In patients who cannot describe their pain or communicate that they are experiencing pain, nurses should look for other signs of pain - such as restlessness, agitation, tachycardia, diaphoresis, pallor, etc.
Recording the vital signs
So far, this chapter has described in detail the processes involved in measuring a patient's vital signs. Once these have been measured, the information must be documented so that it can be used to: (1) assess the patient's condition, and (2) inform the care which is appropriate for that patient. As you saw in a previous chapter of this module, there are a variety of different ways that data can be recorded, and this generally differs between clinical settings and organisations; nurses are encouraged to familiarise themselves with the documentation strategies used in the organisation where they work. Regardless of how data is recorded, however, documentation must be complete, accurate, concise, legible and free from bias. You should revise the principles of documenting health observation and assessment data from the earlier chapter of this module, if required.
Often in the United Kingdom, a patient's vital signs are recorded using early warning score tools. These pieces of documentation allow a nurse to graphically represent a patient's vital sign measurements to identify changes over time, and to calculate simple scores which describe a patient's risk of deterioration into serious illness. Early warning score tools may also provide a nurse with information about how they should respond if they identify that a patient's vital signs are outside the expected ranges - for example, by increasing the frequency of monitoring, by requesting a medical review or by initiating an emergency call.
Interpreting the vital signs
Once you have measured and recorded a patient's vital signs, it is important that you are able to analyse and interpret the data you have collected. Essentially, this means attempting to understand and make sense of this data, based on the patient's physiological condition. Remember: it is important that nurses use critical thinking to interpret the entire clinical picture of the individual patient with whom they are working. Let's consider a case study example:
Elizabeth is a graduate nurse working in the Accident and Emergency Department (A&E) of a large tertiary hospital in London. She is caring for a young man, Luke, who has been transported by road ambulance following a high-speed motor vehicle accident. Luke has an open, mid-shaft femoral fracture which is bleeding heavily.
Whilst receiving handover from the paramedics who attended the scene, Elizabeth measures Luke's vital signs, finding:
- A HR of 101 beats per minute (high).
- A RR of 18 breaths per minute (high).
- A BP of 60/110 (low).
The paramedics estimate that Luke has lost 1000mL of blood.
Elizabeth analyses and interprets this assessment data. She knows Luke has lost a significant amount of blood, which is likely to result directly in his low BP. Luke's high HR and RR are probably to compensate for his low blood pressure (i.e. his heart beats faster, and he breathes more rapidly, in an attempt to increase perfusion to his organs). Luke's high HR and RR may also be a response to the significant pain he is likely to be experiencing, and also shock at the situation in which he finds himself.
In analysing and interpreting her measurements of Luke's vital signs in this way, Elizabeth can plan effective care for Luke. She also has a baseline which she can use to evaluate the effectiveness of the care provided.
It is important to remember that learning to measure and record a patient's vital signs accurately, and to analyse and interpret the data collected, are skills which comes with practice. As a student and new graduate nurse, it is essential that you take every possible opportunity to practice collecting, recording and interpreting the vital signs of a variety of different patients, in a range of different clinical settings.
As you have seen in this chapter, the measurement and recording of the vital signs is the first step in the process of physically examining a patient - that is, in collecting objective data about a patient's signs (i.e. what the nurse can observe, feel, hear or measure). This chapter began with an introduction to the importance of measuring the vital signs in nursing practice. It went on to describe the measurement of each of the vital signs and the collection of other supporting data (e.g. height, weight, pain score), discussing key strategies and considerations. The chapter then reviewed the processes involved in recording data collected about the vital signs. Finally, the chapter discussed how a nurse should go about interpreting the data they have obtained, to build a clinical picture of the patient and plan for their care. In completing this chapter, you have become equipped with the knowledge and skills you require to accurately measure and record a patient's vital signs.
Now we have reached the end of this chapter, you should be able:
Reference list
Cox, C. (2009). Physical Assessment for Nurses (2nd edn.). West Sussex, UK: Blackwell Publishing, Ltd.
Jensen, S. (2014). Nursing Health Assessment: A Best Practice Approach . London, UK: Wolters Kluwer Publishing.
Wilson, S.F. & Giddens, J.F. (2005). Health Assessment for Nursing Practice (4th edn.). St Louis, MI: Mosby Elsevier.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
Content relating to: "diagnosis"
Once a patient has been diagnosed, a plan of care should be actioned to include further diagnostic testing, medications, referrals, and follow-up care. Patient education should also be provided regarding diagnosis, exercise, diet, medicines, and warning signs of medication and diagnoses.
Related Articles
Improving men’s awareness of the early symptoms of prostate cancer
Question What can nurses do improve men’s awareness of the early symptoms of prostate cancer? Answer The actor Ben Stiller has revealed in an article in The Daily Telegraph (The Daily Telegraph, 201...
Hyperbilirubinemia Commonality, Physiology and Diagnosis
Hyperbilirubinemia Scholarly Paper Perinatal: Labour, Delivery and Newborn Care Hyperbilirubinemia or neonatal jaundice is a commonly occurring condition in newbo...
Osteoarthritis Diagnosis and Care Plan
The patient is suffering from general osteoarthritis, muscle weakness, abnormal of gal, spinal stenosis, chronic pain neck, benign hypertension, Alzheimer, dementia with behavior disturbance, depressive disorder NEC, and myopia....

In order to continue enjoying our site, we ask that you confirm your identity as a human. Thank you very much for your cooperation.
NTI Recorded Session NTI23299
Vital Lessons: A Case-Based Approach to Abnormal Vital Signs
Author(s): Megan Vennero
Activity Message
Get ce message.
Contact Hours 1.00
CERP A 1.00
Expires Nov 15, 2026
Topics: Monitoring
Population: Adult
Role: Staff
Add to Collection
Added to Collection
Activity Summary
Required reading for all learners: Implicit Bias impacts patient outcomes
- Describe an algorithmic approach to assessing abnormal vital signs.
- Articulate a focused differential based in part on specific vital signs.
- Apply knowledge gained in this presentation to interactive clinical case studies.
Continuing Education Disclosure Statement
Learners must attend/view/read the entire activity, read Implicit Bias impacts patient outcomes , and complete the associated evaluation to be awarded the contact hours or CERP. No partial credit will be awarded.
Accreditation
The American Association of Critical-Care Nurses is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center's Commission on Accreditation.
Provider approved by the California Board of Registered Nursing, Provider number CEP 1036, for 1.00 contact hours.
Accreditation refers to recognition of continuing education only and does not imply AACN, ANCC, or CBRN approval or endorsement of any commercial products discussed or displayed in conjunction with this educational activity.
Any relevant relationship between an ineligible company and an individual with the ability to influence clinical content will be identified by the Nurse Planner within the activity. Any relevant relationship between an ineligible company and an individual with the ability to influence clinical content has been mitigated.
AACN programming meets the standards for most states that require mandatory continuing education contact hours for license and/or certification renewal. AACN recommends consulting with your state board of nursing or credentialing organization before submitting CE to fulfill continuing education requirements.
Continuing Education Activities are nonrefundable.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection
- PMC10946594

Vital sign assessment and nursing interventions in medical and surgical patients with rapid response system triggers
Julie considine.
1 School of Nursing and Midwifery and Centre for Quality and Patient Safety Research in the Institute for Health Transformation, Deakin University, Geelong Australia
2 Centre for Quality and Patient Safety Research – Eastern Health Partnership, Box Hill Australia
Alison M. Hutchinson
3 Centre for Quality and Patient Safety Research – Barwon Health Partnership, Geelong Australia
Imogen Mitchell
4 Research and Academic Partnerships, Canberra Health Services, Canberra Australian Capital Territory, Australia
5 Australian National University College of Health and Medicine, Canberra Australian Capital Territory, Australia
Shalika Bohingamu Mudiyanselage
6 School of Health and Social Development, Deakin Health Economics, Institute for Health Transformation, Faculty of Health, Deakin University, Geelong Australia
Mohammadreza Mohebbi
7 Biostatistics Unit, Faculty of Health, Deakin University, Burwood Victoria, Australia
Jennifer J. Watts
Tracey bucknall.
8 Centre for Quality and Patient Safety Research – Alfred Health Partnership, Melbourne Australia
Associated Data
Table S2: STROBE Statement—Checklist of items that should be included in reports of cohort studies (von Elm et al., 2007 )
Table S3: Study ward charactersitics
Table S4: Examples of recoding of ‘other’ nursing interventions from free text data
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
To explore vital sign assessment (both complete and incomplete sets of vital signs), and escalation of care per policy and nursing interventions in response to clinical deterioration.
This cohort study is a secondary analysis of data from the Prioritising Responses of Nurses To deteriorating patient Observations cluster randomised controlled trial of a facilitation intervention on nurses' vital sign measurement and escalation of care for deteriorating patients.
The study was conducted in 36 wards at four metropolitan hospitals in Victoria, Australia. Medical records of all included patients from the study wards during three randomly selected 24‐h periods within the same week were audited at three time points: pre‐intervention (June 2016), and at 6 (December 2016) and 12 months (June 1017) post‐intervention. Descriptive statistics were used to summarise the study data, and relationships between variables were examined using chi‐square test.
A total of 10,383 audits were conducted. At least one vital sign measurement was documented every 8 h in 91.6% of audits, and a complete set of vital signs was documented every 8 h in 83.1% of audits. There were pre‐Medical Emergency Team, Medical Emergency Team or Cardiac Arrest Team triggers in 25.8% of audits. When triggers were present, a rapid response system call occurred in 26.8% of audits. There were 1350 documented nursing interventions in audits with pre‐Medical Emergency Team ( n = 2403) or Medical Emergency Team triggers ( n = 273). One or more nursing interventions were documented in 29.5% of audits with pre‐Medical Emergency Team triggers and 63.7% of audits with Medical Emergency Team triggers.
- When rapid response system triggers were documented, there were gaps in escalation of care per policy; however, nurses undertook a range of interventions within their scope of practice in response to clinical deterioration.
Relevance to Clinical Practice
Medical and surgical ward nurses in acute care wards frequently engage in vital sign assessment. Interventions by medical and nurgical nurses may occur prior to, or in parallel with calling the rapid response system. Nursing interventions are a key but under‐recognised element of the organisational response to deteriorating patients.
Implications for the profession and/or patient care
Nurses engage in a range of nursing interventions to manage deteriorating patients, (aside from rapid response system activation) that are not well understood, nor well described in the literature to date.
- This study addresses the gap in the literature regarding nurses' management of deteriorating patients within their scope of practice (aside from RRS activation) in real world settings.
- The results of this research are relevant to nurses working on medical and surgical wards.
Reporting Method
The trial was reported according to the Consolidated Standards of Reporting Trials extension for Cluster Trials recommendations, and this paper is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology Statement.
Patient or Public Contribution
No Patient or Public Contribution.
What does this paper contribute to the wider global clinical community?
- This study highlights the important role of nurses in the management of deteriorating patients within their scope of practice.
- Nurses engage in a range of nursing interventions to manage deteriorating patients (aside from rapid response system activation) that are not well understood, nor well described in the literature to date.
1. INTRODUCTION
Recognising and responding to clinical deterioration is a core nursing responsibility. In Australia, recognising and responding to clinical deterioration in acute care hospitals is informed by two key documents. First, the National Consensus Statement (ACSQHC, 2010 ) describes the essential elements for timely recognition of, and response to, deteriorating patients, and second, the National Safety and Quality Health Service Standards (ACSQHC, 2011 ) required for hospital accreditation, in particular, relating to recognising and responding to acute clinical deterioration. Rapid response systems (RRSs) are a core patient safety strategy aimed at facilitating recognition of deteriorating patients, and escalation of care so that clinical deterioration can be managed at the point of care. As nurses have the most direct contact time with patients, they are commonly the first clinician to recognise clinical deterioration (Considine & Currey, 2015 ). Nurses are also the highest RRS users so the success of hospital RRSs is highly dependent on nurses' accuracy of patient assessment, interpretation of data and escalation of care when clinical deterioration is identified (Considine & Currey, 2015 ).
There are numerous published studies of vital sign assessment by nurses (Brekke et al., 2019 ; Bucknall et al., 2022 ; Mok, Wang, & Liaw, 2015 ) and nurses' compliance with RRS activation in patients with vital sign abnormalities (Bingham et al., 2015 ; Bucknall et al., 2022 ; Bucknall, Jones, Bellomo, Staples, & for the RESCUE Investigators, 2013 ; Guinane et al., 2013 ; Shearer et al., 2012 ). One of the largest studies was the Prioritising Responses of Nurses To deteriorating patient Observations (PRONTO) pragmatic cluster randomised controlled trial that tested the effect of a facilitation intervention on nurses' vital sign measurement, interpretation, and escalation of care for deteriorating patients (Bucknall et al., 2022 ).
The outcomes of interest were as follows: (i) vital sign assessments at least 8‐hourly on every patient; (ii) escalation of care per policy for patients with vital sign abnormalities; and (iii) implementation of appropriate nursing interventions in response to clinical deterioration (ACSQHC 2010). The control wards ( n = 18) received standard dissemination of hospital policy requirements to achieve the outcomes of interest. This comprised distribution of the National Consensus Statement (ACSQHC 2010) and relevant National Safety and Quality Health Service Standards (ACSQHC 2011) by the Nurse Managers at staff meetings and via email, and notification of free online educational courses about recognition and response to deteriorating patients (Bucknall et al., 2017 ). The intervention wards ( n = 18) had an external facilitator across hospitals, an internal hospital facilitator (HFLIP) and two ward facilitators (WFLIPs) per ward for 6 months who used facilitation methods to address barriers and leverage enablers to achieve the desired outcomes (Bucknall et al., 2022 ). There were no significant differences in any of the three outcomes of interest between intervention and control wards at 6 or 12 months post‐intervention (Bucknall et al., 2022 ).
It may be argued that the focus on nurses' compliance with vital sign measurement and RRS activation in patients with vital sign abnormalities is a simplistic view of nursing practice. It is possible that the nature of deterioration (such as the specific RRS trigger breached and the degree of abnormality) and nursing interventions for the management of deteriorating patients influence whether nurses do or do not activate the RRS. Whilst there are a number of studies detailing the interventions undertaken by the rapid response team (Flabouris et al., 2010 ; Jung et al., 2016 ; Mullins & Psirides, 2016 ; Silva et al., 2016 ; White et al., 2016 ), how nurses manage deteriorating patients within their scope of practice (aside from RRS activation) in real world settings is poorly understood.
The aims of this study were to explore: (i) the type and frequency of vital sign assessment (both complete and incomplete sets of vital signs); (ii) the relationship between escalation of care per policy and specific RRS triggers; and (iii) the relationship between escalation of care per policy and nursing interventions in response to clinical deterioration.
For the purpose of this study, escalation of care per policy was defined as escalation of care to the pre‐Medical Emergency Team (pre‐MET), Medical Emergency Team (MET) or Cardiac Arrest Team (CAT) in response to pre‐determined organisational criteria for each RRS tier (pre‐MET call for pre‐MET criteria, MET call for MET criteria and CAT call for cardiac arrest; Table S1 ). A complete set of vital signs was defined as documentation of respiratory rate, oxygen saturation, heart rate, blood pressure, conscious state and temperature (ACSQHC, 2010). Clinician concern was defined as care having been escalated without documented vital sign abnormalities.
2.1. Design
This cohort study was a secondary analysis of data from the PRONTO cluster randomised controlled trial, the methodology and results of which are reported elsewhere [references redacted]. The trial was reported according to the Consolidated Standards of Reporting Trials extension for Cluster Trials (CONSORT) recommendations (Campbell et al., 2012 ), and this paper is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement (von Elm et al., 2007 ) (Table S2 ). This study was approved by Consultative Council for Clinical Trial Research (CCCTR) Victorian Streamlined Ethical Review Process (SERP) [HREC/16/ALFRED/25] and Deakin University [2016–248] (Bucknall et al., 2022 ).
2.2. Setting
The study was conducted in 36 wards at four university‐affiliated, metropolitan hospitals in Victoria, Australia, each with over 400 beds and providing acute and specialist services (Bucknall et al., 2017 ; Bucknall et al., 2022 ). The wards were a mix of medical and surgical wards comprising 21–46 beds per ward. The characteristics of the included wards are shown in Table S3 . None of the study hospitals had an electronic medical record in place.
All four hospitals had a three‐tier RRS consisting of pre‐MET (single trigger), MET (single trigger) and CAT (Table S1 ). The CAT and MET were medically‐led teams of intensive care unit (ICU) clinicians who responded to deteriorating ward‐based patients, whilst the pre‐MET response was by ward‐based doctors and senior ward nurses. In addition, all four hospitals had paper‐based, colour coded observation and response charts that provided nurses with a visual prompt and guidance in terms of the appropriate organisational response, when documenting vital signs fulfilling pre‐MET or MET triggers. Nurse‐to‐patient ratios on all wards were 1:4 on morning and afternoon shifts and 1:8 overnight. Nurse staffing was a combination of registered nurses (Bachelor‐prepared) and enrolled nurses (Diploma‐prepared, working under the supervision of registered nurses).
2.3. Sample
All inpatients from the PRONTO study wards (medical and surgical) during the data collection periods were included. Patients from critical care, emergency, paediatrics, maternity, perioperative and psychiatric areas were excluded because these areas used alternative response systems for deteriorating patients. All study wards were subject to the same RRS criteria and governance, and nursing scope of practice; thus, the opportunities for escalation of care per policy and nursing interventions for deteriorating patients were the same for all patients.
2.4. Data collection
Medical record audits were conducted on all included patients at three time points (T0, T1, T2): pre‐intervention (T0), and at 6 (T1) and 12 months (T2) post‐intervention. Data were collected during three randomly selected 24‐hour periods within the same week in June 2016 (T0), December 2016 (T1) and June 2017 (T2); therefore, a single patient could be represented on multiple audit days (Bucknall et al., 2022 ). An electronic Case Report Form (eCRF) was used to collect study data. At each audit, documented vital sign data were collected: for vital signs fulfilling organisational pre‐MET and MET triggers (tailored to each organisation as per Table S1 ), data relating to any escalation of care per hospital policy were also collected. Data were collected by research assistants who received specific training on the electronic data collection tool and accompanying data dictionary. Inter‐rater reliability testing was established by independent double auditing across sites until Kappa >0.95 was achieved, with a minimum of 10 medical records audited per research assistant. In addition, project manager who was a registered nurse conducted study monitoring on a random sample of 100 patient charts across four sites to ensure data accuracy (Bucknall et al., 2017 ).
Fifteen nursing interventions were nominated apriori by the research team based on their clinical nursing expertise, hospital policies and nursing scope of practice. The apriori interventions were respiratory assessment, adjust oxygen therapy, reposition patient, withhold medication, administer medications as ordered, electrocardiography, encourage oral fluids, heated blankets, cardiovascular assessment, Glasgow Coma Score assessment, pain assessment, commence fluid balance chart, assess drainage fluid, reassess vital signs and other. If ‘other’ was selected, the research assistants were to add free text detail. Analysis of free text data by one nursing researcher (JC) resulted in six additional interventions based on frequencies: blood cultures ( n = 31), deep breathing and coughing ( n = 29), measure blood glucose level ( n = 29), notify medical staff ( n = 11), intravenous fluids ( n = 6) and pathology testing ( n = 5). The codes were ratified by the chief investigator (TB): examples of the free text coding process are shown in Table S4 .
2.5. Data analysis
Data were analysed using SPSS Version 29.0. Descriptive statistics were used to summarise the study data. As data were not normally distributed (according to the Kolmogorov–Smirnov test), medians and interquartile ranges (IQRs) are presented. Relationships between variables were examined using chi‐square test, and statistical significance was indicated by p < 0.05. False‐discovery rate (FDR) was corrected by using the Benjamini–Hochberg approach (Benjamini & Hochberg, 1995 ) to mitigate the risk of type‐I error inflation from multiple comparisons; therefore, the cut‐off for statistical significance was more conservative than the usual 0.05. Pre‐MET and MET triggers were categorised as present or not present according to organisational thresholds detailed in Table S1 .
A total of 10,383 audits were conducted across 3 days in a single week in June 2016 ( n = 3370), December 2016 ( n = 3535) and June 2017 ( n = 3478). As there were the same patients ( n = 6065) present during multiple audits, results are presented at the audit level rather than the patient level.
3.1. Vital sign assessment
Of the 10,383 audits, at least one vital sign measurement was documented every 8 h in 91.6% of audits ( n = 9514) and a complete set of vital signs was documented every 8 h in 83.1% ( n = 8631) of audits. In 86.8% of audits ( n = 9015), there was evidence of further vital sign assessments in addition to the mandated 8‐hourly assessments: the median number of extra vital sign assessments was 2 (IQR = 1–3). The most frequently missing vital signs were temperature (2.7%, n = 279) and conscious state (2.7%, n = 278). The remaining vital signs had few missing values: respiratory rate (1.4%, n = 150), systolic blood pressure (1.2%, n = 121), heart rate (1.1%, n = 119) and oxygen saturation (1.1%, n = 116).
3.2. Escalation of care per policy in audits with RRS triggers
Of the 10,383 audits, 25.8% ( n = 2680) had evidence of pre‐MET, MET or CAT triggers (pre‐MET 23.1%, n = 2403; MET 2.6%, n = 273 and CAT 0.3%, n = 4). When RRS triggers were present, a documented call to the appropriate tier of the RRS was evident in 26.8% of audits (Table 1 ).
Frequency of rapid response system triggers and escalation of care per policy.
| Rapid response system tier | Fulfilled RRS triggers | No escalation of care per policy | Escalation of care per policy | ||
|---|---|---|---|---|---|
| % | % | ||||
| Pre‐MET | 2403 | 1771 | 73.7 | 632 | 26.3 |
| MET | 273 | 186 | 68.1 | 87 | 31.9 |
| CAT | 4 | 0 | 0 | 4 | 100 |
When pre‐MET triggers were present ( n = 2403 audits), escalation of care per policy (pre‐MET call) was significantly more likely when hypotension (23.3% vs. 13.3%, FDR < 0.05), hyperthermia (18.5% vs. 3.1%, FDR < 0.05), hypertension (17.1% vs. 6.2%, FDR < 0.05), tachypnoea (9.8% vs. 5.1%, FDR < 0.05) and clinical concern (8.1% vs. 0.2%, FDR < 0.05) were present. Pre‐MET escalation of care was significantly less likely when there was hypoxaemia (7.1% vs. 16.4%, FDR < 0.05), bradycardia (4.9% vs. 7.9%, FDR = 0.012), decreased conscious state (3.5% vs. 16.4%, FDR < 0.05) and hypothermia (3.3% vs. 15.4%, FDR < 0.05) (Table 2 ). Three audits with documented clinical concern and no escalation of care also had documented hypotension ( n = 2) or bradycardia ( n = 1). Of the 51 audits with documented clinical concern and pre‐MET escalation of care, 50 had no documented vital sign abnormalities and one had documented tachycardia. Examples of pre‐MET clinical concern were decreased breath sounds, agitation, chest pain, epistaxis, family concern, falls and rectal bleeding.
Escalation of care per policy versus pre‐MET or MET triggers.
| Audits with pre‐MET triggers | Escalation of care per policy | ||||||
|---|---|---|---|---|---|---|---|
| No pre‐MET call ( = 1771) | Pre‐MET call ( = 632) | OR | 95% CI | ||||
| n | % | n | % | ||||
| Patient characteristics | |||||||
| Female gender | 838 | 47.3 | 296 | 46.6 | 0.835 | 0.981 | 0.81–1.17 |
| Limitation of medical treatment orders | 563 | 31.8 | 176 | 27.8 | 0.064 | 0.827 | 0.68–1.01 |
| Emergency admission (vs. elective) | 1559 | 88.1 | 530 | 83.9 | 0.007 | 0.703 | 0.54–0.91 |
| Specific triggers | |||||||
| Bradypnoea | 16 | 0.9 | 4 | 0.6 | 0.520 | 0.698 | 0.23–2.01 |
| Tachypnoea | 90 | 5.1 | 62 | 9.8 | <0.001 | 1.913 | 1.36–2.68 |
| Hypoxaemia | 290 | 16.4 | 45 | 7.1 | <0.001 | 0.391 | 0.28–0.54 |
| Bradycardia | 140 | 7.9 | 31 | 4.9 | 0.012 | 0.601 | 0.40–0.89 |
| Tachycardia | 327 | 18.5 | 116 | 18.4 | 0.760 | 0.964 | 0.76–1.22 |
| Hypertension | 110 | 6.2 | 108 | 17.1 | <0.001 | 3.110 | 2.34–4.13 |
| Hypotension | 235 | 13.3 | 147 | 23.3 | <0.001 | 1.785 | 0.42–2.24 |
| Decreased conscious state | 291 | 16.4 | 22 | 3.5 | <0.001 | 0.183 | 0.12–0.28 |
| Hyperthermia | 55 | 3.1 | 117 | 18.5 | <0.001 | 6.958 | 4.98–9.71 |
| Hypothermia | 273 | 15.4 | 21 | 3.3 | <0.001 | 0.188 | 0.12–0.29 |
| Clinical concern | 3 | 0.2 | 51 | 8.1 | <0.001 | 51.702 | 16.07–166.28 |
| Audits with MET triggers | No MET call ( = 186) | MET call ( = 87) | |||||
| % | % | ||||||
| Patient characteristics | |||||||
| Female gender | 96 | 51.6 | 38 | 43.7 | 0.222 | 0.727 | 0.46–1.21 |
| Limitation of medical treatment orders | 67 | 60.4 | 44 | 39.6 | 0.023 | 1.817 | 1.08–3.04 |
| Emergency admission (vs. elective) | 132 | 68.6 | 74 | 31.4 | 0.569 | 0.808 | 0.38–1.68 |
| Specific triggers | |||||||
| Tachypnoea | 20 | 10.8 | 9 | 10.3 | 0.816 | 0.907 | 0.39–2.07 |
| Hypoxaemia | 53 | 28.5 | 15 | 17.2 | 0.045 | 0.523 | 0.27–0.99 |
| Bradycardia | 8 | 4.3 | 0 | 0.0 | 0.058 | 0.672 | 0.62–0.73 |
| Tachycardia | 17 | 9.1 | 24 | 27.6 | <0.001 | 3.787 | 1.91–7.51 |
| Hypertension | 0 | 0.0 | 2 | 2.3 | 0.101 | 0.314 | 0.26–0.37 |
| Hypotension | 79 | 42.5 | 22 | 25.3 | 0.006 | 0.458 | 0.26–0.81 |
| Decreased conscious state | 9 | 4.8 | 12 | 13.8 | 0.014 | 3.147 | 1.27–7.78 |
| Clinical concern | 0 | 0.0 | 10 | 11.5 | <0.001 | 24.02 | 3.02–190.92 |
OR, odd ratio; CI, confidence interval.
Of the audits with MET triggers ( n = 273), escalation of care per policy (MET call) was significantly higher when tachycardia (27.6% vs. 9.1%, FDR < 0.05), decreased conscious state (13.8% vs. 4.8%, FDR = 0.014) and clinical concern (11.5% vs. 0.5%, FDR < 0.05) were present and significantly lower in the presence of hypotension (42.5% vs. 25.3%, FDR = 0.007) (hypoxaemia did not retain statistical significance following Benjamini–Hochberg correction). Of the ten audits with documented clinical concern and MET escalation of care, three had clinical concern (chest pain) documented in addition to documented tachycardia, one had documented general concern, tachycardia and decreased conscious state, and six had no documented vital sign abnormalities but had documented concerns regarding falls, uncontrolled pain and agitation. Patients who had emergency (versus elective) admissions had significantly less escalation of care per policy if pre‐MET triggers were present (83.9% vs. 88.1, FDR = 0.007) (Table 2 ).
3.3. Escalation of care per policy and specific nursing interventions
There was no significant difference in nursing interventions for pre‐MET (51.0% vs. 49.0%, p = 0.788, OR = 1.024, 95%CI: 0.86–1.22) or MET triggers (59.2% vs. 67.8%, p = 0.140, OR = 0.689, 95%CI: 0.42–1.13) between intervention and control wards. Overall, there were 1350 documented nursing interventions in audits with pre‐MET ( n = 2403) or MET triggers ( n = 273) (Table 3 ).
Nursing interventions associated with presence of pre‐MET or MET triggers versus escalation of care per policy.
| Documented nursing interventions | Presence of pre‐MET triggers ( = 2403 audits) | Presence of MET triggers ( = 273 audits) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total number of nursing interventions ( = 1034) | No pre‐MET call ( = 1771) | Pre‐MET call ( = 632) | OR | 95% CI | Total number of nursing interventions ( = 316) | No MET call ( = 186) | MET call ( = 87) | OR | 95% CI | |||||||||
| % | % | % | % | % | % | |||||||||||||
| Administer medications as ordered | 209 | 20.2 | 69 | 3.9 | 140 | 22.2 | <0.001 | 7.015 | 5.17–9.52 | 14 | 4.4 | 8 | 4.3 | 6 | 6.9 | 0.385 | 1.648 | 0.54–4.90 |
| Adjust oxygen therapy | 162 | 15.7 | 126 | 7.1 | 36 | 5.7 | 0.221 | 0.788 | 0.24–1.15 | 52 | 16.5 | 39 | 21.0 | 13 | 14.9 | 0.237 | 0.662 | 0.33–1.32 |
| Other | 158 | 15.3 | 80 | 4.5 | 78 | 12.3 | <0.001 | 2.974 | 2.14–4.12 | 55 | 17.4 | 23 | 12.4 | 32 | 36.8 | <0.001 | 4.123 | 2.22–7.64 |
| Reassess vital signs | 120 | 11.6 | 73 | 4.1 | 47 | 7.4 | 0.001 | 1.86 | 1.28–2.72 | 36 | 11.4 | 27 | 14.5 | 9 | 10.3 | 0.343 | 0.679 | 0.30–1.51 |
| Perform electrocardiography | 85 | 8.2 | 7 | 0.4 | 78 | 12.3 | <0.001 | 35.460 | 16.27–77.29 | 36 | 11.4 | 10 | 5.4 | 26 | 29.9 | <0.001 | 7.50 | 3.42–16.45 |
| GCS assessment | 67 | 6.5 | 54 | 3.0 | 13 | 2.1 | 0.193 | 0.667 | 0.36–1.23 | 29 | 9.2 | 2 | 1.1 | 27 | 31.0 | <0.001 | 41.4 | 9.56–179‐26 |
| Administer oral fluids | 63 | 6.1 | 21 | 1.2 | 42 | 6.6 | <0.001 | 5.929 | 3.48–10.09 | 18 | 5.7 | 13 | 7.0 | 5 | 5.7 | 0.700 | 0.811 | 0.28–2.35 |
| Reposition patient | 36 | 3.5 | 18 | 1.0 | 18 | 2.8 | 0.001 | 2.853 | 4.17–5.52 | 25 | 7.9 | 16 | 8.6 | 9 | 10.3 | 0.642 | 1.226 | 0.25–2.89 |
| Blood cultures | 30 | 2.9 | 7 | 0.4 | 23 | 3.6 | <0.001 | 9.517 | 4.06–22.29 | 1 | 0.3 | 1 | 0.5 | 0 | 0.0 | 1.000 | N/A | N/A |
| Respiratory assessment | 27 | 2.6 | 20 | 1.1 | 7 | 1.1 | 0.964 | 0.980 | 0.41–2.33 | 3 | 0.9 | 3 | 1.6 | 0 | 0.0 | 0.554 | N/A | N/A |
| Deep breathing & coughing | 24 | 2.3 | 20 | 1.1 | 4 | 0.6 | 0.281 | 0.558 | 0.19–1.64 | 5 | 1.6 | 5 | 2.7 | 0 | 0.0 | 0.181 | N/A | N/A |
| Withhold medication | 11 | 1.1 | 2 | 0.1 | 9 | 1.4 | <0.001 | 12.770 | 2.75–59.27 | 4 | 1.3 | 4 | 2.2 | 0 | 0.0 | 0.310 | N/A | N/A |
| Notify medical staff | 8 | 0.8 | 2 | 0.1 | 6 | 0.9 | 0.005 | 8.478 | 1.70–42.11 | 3 | 0.9 | 2 | 1.1 | 1 | 1.1 | 1.000 | 1.070 | 0.09–11.96 |
| Cardiovascular assessment | 7 | 0.7 | 2 | 0.1 | 5 | 0.8 | 0.016 | 7.049 | 1.36–36.28 | 2 | 0.6 | 1 | 0.5 | 1 | 1.1 | 0.537 | 2.15 | 0.13–34.79 |
| IV fluids | 4 | 0.4 | 1 | 0.1 | 3 | 0.5 | 0.058 | 8.442 | 0.88–81.30 | 2 | 0.6 | 2 | 1.1 | 0 | 0.0 | 1.000 | N/A | N/A |
| Pain assessment | 4 | 0.4 | 2 | 0.1 | 2 | 0.3 | 0.284 | 2.806 | 0.39–19.96 | 1 | 0.3 | 0 | 0.0 | 1 | 1.1 | 0.319 | N/A | N/A |
| Pathology testing | 4 | 0.4 | 1 | 0.1 | 3 | 0.5 | 0.058 | 8.442 | 0.87–81.30 | 1 | 0.3 | 1 | 0.5 | 0 | 0.0 | 1.000 | 0.680 | 0.63–0.74 |
| Measure blood glucose level | 3 | 0.3 | 0 | 0.0 | 3 | 0.5 | 0.018 | N/A | N/A | 26 | 8.2 | 2 | 1.1 | 24 | 27.6 | <0.001 | 35.048 | 8.05–152‐52 |
| Assess drainage fluid | 1 | 0.1 | 1 | 0.1 | 0 | 0.0 | 1.000 | N/A | N/A | 3 | 0.9 | 2 | 1.1 | 1 | 1.1 | 1.000 | 1.070 | 0.09–11.96 |
| Commence fluid balance chart | 1 | 0.1 | 0 | 0.0 | 1 | 0.2 | 0.263 | N/A | N/A | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | N/A | N/A | N/A |
| Provide heated blankets | 10 | 1.0 | 7 | 0.4 | 3 | 0.5 | 0.729 | 1.201 | 0.31–4.66 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | N/A | N/A | N/A |
Abbreviations: OR, odd ratio CI = confidence interval.
3.3.1. Audits with pre‐MET triggers
One or more nursing interventions were documented in 29.5% ( n = 710/2403) of audits with pre‐MET triggers. The median number of nursing interventions in audits with pre‐MET triggers was 1 (IQR = 1–2). The most common nursing interventions associated with pre‐MET triggers were medication administration (20.2%), adjustment to oxygen therapy (15.7%) and vital sign reassessment (11.6%). Nursing interventions were significantly more likely when there were pre‐MET triggers and care was escalated per policy (55.1%, n = 348/632) compared to pre‐MET triggers and no care escalation (24.0%, n = 362/ 1771) ( p < 0.001). When pre‐MET triggers were present, the following nursing interventions were significantly more likely when care was escalated per policy: medication administration, vital sign reassessment, electrocardiography, oral fluid administration, patient repositioning, blood culture collection, withholding of medication, medical staff notification, cardiovascular assessment and blood glucose measurement (Table 3 ).
3.3.2. Audits with MET triggers
One or more nursing interventions were documented in 63.7% ( n = 174/273) of audits with MET triggers. The median number of nursing interventions in audits with MET triggers was 1 (IQR = 1–3). The most common nursing interventions associated with MET triggers were adjustment to oxygen therapy (16.5%), electrocardiography (11.4%) and vital sign reassessment (11.4%). Nursing interventions were significantly more likely when there were MET triggers and care was escalated per policy (78.2%, n = 68/87) compared to MET triggers and no care escalation (57.0%, n = 106/186) ( p < 0.001). When MET triggers were present, the following nursing interventions were significantly more likely when care was escalated per policy: electrocardiography, Glasgow Coma Score assessment and blood glucose measurement (Table 3 ).
4. DISCUSSION
This study had four major findings: there were high levels of 8‐hourly vital sign assessment and documentation of complete sets of vital signs as per policy; there was low compliance with escalation of care per policy in the presence of pre‐MET, MET and CAT triggers; specific pre‐MET and MET triggers influenced whether care was escalated per policy; and nursing interventions were common when pre‐MET or MET triggers were present. These major findings will be discussed in the sections to follow.
First, 91.6% of audits had at least one vital sign assessment every 8 h and 83.1% of audits had a complete set of vital signs documented every 8 h. Our findings are different to those of other studies that report proportions of vital signs assessments with one or more missing vital signs ranging from zero to 41% (Bleyer et al., 2011 ; Cahill et al., 2011 ; Chen et al., 2009 ). The implementation of national standards for frequency of vital sign assessment, making 8‐hourly vital sign assessment a minimum standard for hospital accreditation, use of human factors in the design of observation charts, and educational interventions aimed at increasing recognition of clinical deterioration and RRS activation, may be possible explanations for this finding (ACSQHC, 2010, 2011). The most frequently missing vital signs in our study were temperature (2.7%, n = 279) and conscious state (2.7%, n = 278).
Bleyer et al. ( 2011 ) also reported temperature as the most common missing vital sign, albeit at a much higher rate (17.8%) than in our study. Acknowledging there were low levels of missing temperature documentation in our study, it may be hypothesised that the need to engage in increased activity (e.g. sourcing a tympanic thermometer) negatively influenced measurement and documentation of temperature. A number of authors report respiratory rate as the least documented vital sign (Cahill et al., 2011 ; Cardona‐Morrell et al., 2016 ; Chen et al., 2009 ), however, in our study, only 1.4% of audits were missing documentation of respiratory rate. The importance of respiratory rate as a sensitive and specific vital sign indicator of serious illness has gained increased recognition in the decade prior to the trial (Cretikos et al., 2008 ), which may in part have influenced this finding.
Second, escalation of care per policy occurred in only one in four audits with pre‐MET, MET and CAT triggers. Pre‐MET, MET and CAT triggers were present in 25.8% of audits in this study, and pre‐MET triggers were more common than MET triggers (23.1% vs 2.6%). Failure to escalate care per policy occurred in 73.7% of audits with pre‐MET triggers and 68.1% of audits with MET triggers. The majority of studies to date have focused on either pre‐MET or MET RRS tiers; there are few published studies to date that examine the pre‐MET and MET RRS tiers as a continuum within the same patients (Bingham et al., 2015 ; Flabouris et al., 2015 ). Our findings are reflective of those of Bingham et al. ( 2015 ) and Flabouris et al. ( 2015 ) whose single‐site studies showed that pre‐MET triggers are more common than MET triggers, presumably because of the wider thresholds of pre‐MET triggers. In these studies, failure to escalate care per policy for pre‐MET and MET triggers were measured using different methods, limiting direct comparisons between studies. In 24‐h point prevalence studies, failure to escalate care per policy when pre‐MET or MET triggers were present ranged from 45.1% (47% pre‐MET and 30% MET triggers) to 50.9% (52.2% pre‐MET triggers and 45.5% MET triggers) (Bingham et al., 2015 ; Flabouris et al., 2015 ). At the patient level, failure to escalate care for pre‐MET or MET triggers during the course of hospital admission was reported in 51.6% of patients (65.0% pre‐MET and 35.3% MET, p < 0.01) (Flabouris et al., 2015 ). At the trigger level, 58.7% of pre‐MET or MET triggers were not escalated (64.7% pre‐MET and 40% MET, no p value reported) (Flabouris et al., 2015 ).
Whilst there were gaps in escalation of care per policy (pre‐MET call for pre‐MET triggers and MET call for MET triggers) in this study, it is possible that nurses used alternative methods of escalation of care to mobilise medical staff to the point of care. It is well documented that nurses commonly escalate care to treating (admitting) teams instead of activating the RRS (Jones et al., 2006 ; Shearer et al., 2012 ). Other studies have shown that nurses used the RRS if they perceived the treating team were not responding appropriately (Bingham et al., 2020 ; Jones et al., 2006 ) and it is also possible that nurses prefer to communicate their concerns to ward medical staff with whom they have a relationship over MET responders who they may not know.
Third, escalation of care per policy varied according to specific pre‐MET or MET triggers. Higher likelihood of escalation of care occurred in the presence of pre‐MET blood pressure derangements, hyperthermia and tachypnoea, and MET triggers tachycardia and decreased conscious state. Other studies also show altered conscious state and tachycardia are the most common MET triggers (Davies et al., 2014 ; Mullins & Psirides, 2016 ) and had zero failure to escalate rates (Flabouris et al., 2015 ). It is possible in our study that pre‐MET escalation of care for tachypnoea, may have resulted in early intervention and circumvented later MET calls for tachypnoea, which has two important implications. First, it may be proposed that nurses are now recognising the importance of tachypnoea as an indicator of deterioration, which is supported by the low rates of missing documentation of respiratory rate (1.4%) in our study and that 87.5% of nurses in another study agreed that the respiratory rate criterion of the RRS had the most benefit (Davies et al., 2014 ). Second, the relationship between pre‐MET escalation of care and interventions in reducing physiological derangement to MET trigger levels warrants further research.
Of concern is failure to escalate care. Pre‐MET hypoxemia, bradycardia, decreased conscious state, and hypothermia, and MET level hypotension were all associated with lower likelihood of pre‐MET or MET call, respectively. There are few published papers that report pre‐MET failure to escalate rates; however, our findings resemble those of Flabouris et al. ( 2015 ) who reported bradycardia (75%) and hypothermia (66.7%) as having the highest failure to escalate rates of all pre‐MET triggers. MET activation failure in the presence of hypotension is reported in other studies and ranges from 32% to 39% (Considine et al., in press ; Flabouris et al., 2015 ). Further, there is conflict in the literature about nurses' perceptions of the importance of blood pressure with as many as 60% of nurses in one study believing (erroneously) that blood pressure changes are the first indicator of clinical deterioration (Mok, Wang, Cooper, et al., 2015 ). Nurses in another study, however, ranked mean arterial pressure as the RRS trigger with the second lowest level of perceived benefit (Davies et al., 2014 ). In our study, there was decreased likelihood of escalation of care when pre‐MET and MET hypoxaemia were present; however, statistical significance did not remain for MET hypoxaemia following Benjamini–Hochberg correction. Failure to escalate care for MET hypoxemia ranged from 36% to 64.7% (Considine et al., in press ; Flabouris et al., 2015 ), and in both of these studies, hypoxemia was the most common trigger associated with failure to activate the MET Again, there are conflicting reports in the literature with 60% of nurses relying on oxygen saturation to evaluate respiratory dysfunction (Mok, Wang, Cooper, et al., 2015 ) but nurses ranking oxygen saturation as the RRS triggers with the lowest perceived benefit (Davies et al., 2014 ). In our study, hyperthermia was associated with increased likelihood of escalation of care in both pre‐MET and MET contexts and this may be due to long‐standing initiatives such as the focus on early recognition and response to sepsis and improvements in processes of care for patients with sepsis. The reasons why some triggers are more or less likely to result in care escalation are unclear and the importance nurses place on specific vital signs as indicators of clinical deterioration should be a focus of future research.
Clinical concern was associated with increased likelihood of escalation of care in both pre‐MET and MET contexts. In our study, almost all of the pre‐MET escalations of care and 60% of MET escalations of care for clinical concern occurred in the absence of documented vital sign abnormalities. Nurses are the most frequent users of the clinician concern RRS criterion and clinician concern is a common reason for MET activation (Douw et al., 2015 ; Flabouris et al., 2015 ; Santiano et al., 2009 ; Silva et al., 2016 ) suggesting that nurses make conscious and deliberate decisions that a patient is deteriorating, even in the absence of MET triggers. A 2020 systematic review showing that nurses used 26 subjective and 147 objective cues to identify changes in patients' clinical states and 94% of the cues used were aimed at recognising clinical deterioration (Burdeu et al., 2021 ) reinforces the notion that recognition of deteriorating patients goes beyond vital signs. Further, it is well documented that nurse concern often precedes vital sign physiological changes in deteriorating patients and there is evidence that RRS activation for clinician concern improves patient outcomes (Douw et al., 2015 ; Santiano et al., 2009 ).
Finally, one third of audits with pre‐MET triggers and two thirds of audits with MET triggers had one or more documented nursing interventions. Further, nursing interventions were significantly more likely in audits where care was escalated per policy, suggesting nurses' response to deteriorating patients is more than simply escalating care using pre‐MET or MET pathways. Evidence of nurse‐initiated interventions for pre‐MET and MET triggers is consistent with nurses' responsibility to respond to deteriorating patients and mitigate risk (Considine & Currey, 2015 ; Massey et al., 2017 ) and reflects findings from other studies that show once clinical deterioration is recognised, nurses actively engage in interventions within their scope of practice (Bingham et al., 2020 ; Donohue & Endacott, 2010 ; Guinane et al., 2013 ).
The nursing management of deteriorating patients within nurses' scope of practice is under‐reported in the literature. Possible explanations for this paucity of literature may be under‐representation of nurses' roles in recognition and response to clinical deterioration at policy level (Considine et al., 2018 ; Sprogis et al., 2021 ), the high focus on nurses' failure to recognise clinical deterioration or lack of compliance with RRS activation (Bingham et al., 2015 ; Bucknall et al., 2013 ; Guinane et al., 2013 ; Shearer et al., 2012 ), or under‐documentation of nursing interventions. Whilst there are a number of studies detailing the interventions implemented by the rapid response team (Flabouris et al., 2010 ; Mullins & Psirides, 2016 ; Silva et al., 2016 ; White et al., 2016 ), how nurses manage deteriorating patients prior to RRS activation or whilst awaiting team arrival is a major knowledge gap worthy of investigation.
4.1. Limitations
The study data were collected using medical record audit so there is the possibility that documentation may not reflect clinical practice behaviours; however, medical records are a legal representation of the care delivered and are commonly used in studies of safety and quality of care. Further, this limitation was moderated by a multisite design and data abstraction performed by trained researchers using a comprehensive data dictionary to optimise data reliability. It is possible that patients with pre‐MET or MET triggers had their care escalated (either per policy or via alternative means) and their clinical deterioration managed appropriately but it was not reflected in the documentation. The relatively small numbers of escalations of care per policy and nursing interventions limited statistical analyses, particularly some of the sub‐analyses, so future studies with larger samples are warranted.
5. CONCLUSION
Medical and surgical ward nurses in acute care wards are meeting or exceeding national standards regarding vital sign assessments. When pre‐MET or MET triggers were documented, there were gaps in escalation of care per policy; however, nurses undertook a range of interventions within their scope of practice in response to clinical deterioration. It was beyond the scope of this study to examine the outcomes from nursing interventions for deteriorating patients in terms of resolution of pre‐MET or MET triggers and RRS activation, but this is an important area for future research. There were relationships between escalation of care per policy and specific pre‐MET and MET triggers: the importance that nurses give to specific physiological parameters and how different triggers impact on nurses' response to clinical deterioration and RRS activation warrants further investigation.
AUTHOR CONTRIBUTIONS
Considine: Conceptualisation, Methodology, Validation, Formal Analysis, Investigation, Data curation, Writing—original draft, Supervision, Project administration, Funding acquisition Hutchinson: Conceptualisation, Methodology, Validation, Formal Analysis, Investigation, Data curation, Writing—original draft, Supervision, Project administration, Funding acquisition Mitchell: Conceptualisation, Methodology, Validation, Formal Analysis, Investigation, Data curation, Writing—original draft, Funding acquisition Bohingamu Mudiyanselage: Formal Analysis, Data curation, Writing—review & editing Mohebbi: Methodology, Validation, Formal Analysis, Investigation, Data curation, Writing—review & editing, Supervision, Project administration, Funding acquisition Watts: Methodology, Validation, Formal Analysis, Data curation, Writing—review & editing, Funding acquisition Bucknall Conceptualisation, Methodology, Validation, Formal Analysis, Investigation, Data curation, Writing—original draft, Supervision, Project administration, Funding acquisition.
FUNDING INFORMATION
The trial was funded by the National Health and Medical Research Council and partner organisations: Alfred Health, Eastern Health, Monash Health, Australian Commission on Safety and Quality in Health Care and SA Health. National Health and Medical Research Council Partnership Project Grant ID1114545.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
The authors have checked to make sure that our submission conforms as applicable to the Journal's statistical guidelines. There is a statistician on the author team (Mohebbi).
Supporting information
Table S1: Rapid Response System criteria per study site
ACKNOWLEDGEMENTS
We would like to acknowledge the following people for their advice, support or participation in the conduct of this research: Gillian Harvey, Ian Graham, Jo Rycroft‐Malone, Bridey Saultry, Mojtaba Lotfaliany, Robin Digby, Mariann Fossum, Daryl Jones, Jonathan Bartlett, Janet Weir‐Phyland, Cheyne Chalmers, David Plunkett, Nicola Dunbar, Lydia Dennett, Gordon Bingham, Jemima Dixon, Deborah Berry, Chipo Danha, Ingrid Brandeggen‐Taylor, Sharon Paul, Lee Hughes, Ellie Duckworth, Kathryn Joseph, Jeanine McKenna, Alice Mercer, Lauren Turner, Winnie Selle, Deborah Lonsdale, Zeann Laggui, Pauline McNamara, Anna Ring, Mary Heyrosa, Jennifer MacLean, Rebecca Cerdor, Melinda Webb, Rebecca Winkler, Stacey Mehri, Margaret Teasdale, Erin Sorrell, Stephanie Tuyau, James‐Norbet Garduce, Linda Shi, Riikka Salmela, Nicole Sanders, Sandra Vilar, Liz Veigas, Truphena Mbati, Jas Nijjar, Emma Sly, Christine Mulyadi, Louise O'Halloran, Megan Schilling, Paige Williams, Sandi Sooriyadasa, Aleisha Clark, Andrea Box, Jenni Hymers, Belinda Moskovitch, Antoinette David, Veronica Lowe, Campbell Cole, Emily Miller, Katelyn Pollard and Steph Jinks. Open access publishing facilitated by Deakin University, as part of the Wiley ‐ Deakin University agreement via the Council of Australian University Librarians.
Considine, J. , Hutchinson, A. M. , Mitchell, I. , Bohingamu Mudiyanselage, S. , Mohebbi, M. , Watts, J. J. , & Bucknall, T. (2023). Vital sign assessment and nursing interventions in medical and surgical patients with rapid response system triggers . Journal of Clinical Nursing , 32 , 7310–7320. 10.1111/jocn.16810 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

DATA AVAILABILITY STATEMENT
- Australian Commission on Safety and Quality in Health Care (ACSQHC) . (2011). National Safety and Quality Health Service Standards . Retrieved from Sydney. Retrieved 1 August 2016 from http://www.safetyandquality.gov.au/publications/national‐safety‐and‐quality‐health‐service‐standards/
- Australian Commission on Safety and Quality in Health Care (ACSQHC) . (2010). National Consensus Statement: essential elements for recognising and responding to clinical deterioration . Retrieved from Sydney. Retrieved 1 August 2016 from http://www.safetyandquality.gov.au/wp‐content/uploads/2012/01/national_consensus_statement.pdf
- Benjamini, Y. , & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing . Journal of the Royal Statistical Society Series B (Methodological) , 57 ( 1 ), 289–300. [ Google Scholar ]
- Bingham, G. , Fossum, M. , Barratt, M. , & Bucknall, T. (2015). Clinical review criteria and medical emergency teams: Evaluating a two‐tier rapid response system . Critical Care and Resuscitation , 17 ( 3 ), 167–173. [ PubMed ] [ Google Scholar ]
- Bingham, G. , Fossum, M. , Hughes, L. , Digby, R. , & Bucknall, T. (2020). The pre‐medical emergency team response: Nurses' decision‐making escalating deterioration to treating teams using urgent review criteria . Journal of Advanced Nursing , 76 ( 8 ), 2171–2181. 10.1111/jan.14433 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bleyer, A. J. , Vidya, S. , Russell, G. B. , Jones, C. M. , Sujata, L. , Daeihagh, P. , & Hire, D. (2011). Longitudinal analysis of one million vital signs in patients in an academic medical center . Resuscitation , 82 ( 11 ), 1387–1392. 10.1016/j.resuscitation.2011.06.033 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brekke, I. J. , Puntervoll, L. H. , Pedersen, P. B. , Kellett, J. , & Brabrand, M. (2019). The value of vital sign trends in predicting and monitoring clinical deterioration: A systematic review . PLoS One , 14 ( 1 ), e0210875. 10.1371/journal.pone.0210875 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bucknall, T. K. , Considine, J. , Harvey, G. , Graham, I. D. , Rycroft‐Malone, J. , Mitchell, I. , Saultry, B. , Watts, J. J. , Mohebbi, M. , Bohingamu Mudiyanselage, S. , Lotfaliany, M. , & Hutchinson, A. (2022). Prioritising responses of nurses to deteriorating patient observations (PRONTO): A pragmatic cluster randomised controlled trial evaluating the effectiveness of a facilitation intervention on recognition and response to clinical deterioration . BMJ Quality & Safety , 31 , 818–830. 10.1136/bmjqs-2021-013785 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bucknall, T. K. , Harvey, G. , Considine, J. , Mitchell, I. , Rycroft‐Malone, J. , Graham, I. D. , Mohebbi, M. , Watts, J. , & Hutchinson, A. M. (2017). Prioritising responses of nurses to deteriorating patient observations (PRONTO) protocol: Testing the effectiveness a facilitation intervention in a pragmatic, cluster‐randomised trial with an embedded process evaluation and cost analysis . Implementation Science , 12 ( 1 ), 85. 10.1186/s13012-017-0617-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bucknall, T. K. , Jones, D. , Bellomo, R. , Staples, M. , & for the RESCUE Investigators . (2013). Responding to medical emergencies: System characteristics under examination (RESCUE). A prospective multi‐site point prevalence study . Resuscitation , 84 ( 2 ), 179–183. 10.1016/j.resuscitation.2012.06.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Burdeu, G. , Lowe, G. , Rasmussen, B. , & Considine, J. (2021). Clinical cues used by nurses to recognize changes in patients' clinical states: A systematic review . Nursing and Health Science , 23 ( 1 ), 9–28. 10.1111/nhs.12778 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cahill, H. , Jones, A. , Herkes, R. , Cook, K. , Stirling, A. , Halbert, T. , Yates, A. , Lal, S. , Gardo, A. , Donnelly, R. , Gattas, D. J. , & Royal Prince Alfred Hospital Clinical Emergency Response System Steering Committee . (2011). Introduction of a new observation chart and education programme is associated with higher rates of vital‐sign ascertainment in hospital wards . BMJ Quality & Safety , 20 ( 9 ), 791–796. 10.1136/bmjqs.2010.045096 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Campbell, M. K. , Piaggio, G. , Elbourne, D. R. , & Altman, D. G. (2012). Consort 2010 statement: Extension to cluster randomised trials . British Medical Journal , 345 ( sep04 1 ), e5661–e5661. 10.1136/bmj.e5661 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cardona‐Morrell, M. , Prgomet, M. , Lake, R. , Nicholson, M. , Harrison, R. , Long, J. , Westbrook, J. , Braithwaite, J. , & Hillman, K. (2016). Vital signs monitoring and nurse–patient interaction: A qualitative observational study of hospital practice . International Journal of Nursing Studies , 56 , 9–16. 10.1016/j.ijnurstu.2015.12.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen, J. , Hillman, K. , Bellomo, R. , Flabouris, A. , Finfer, S. , & Cretikos, M. (2009). The impact of introducing medical emergency team system on the documentations of vital signs . Resuscitation , 80 ( 1 ), 35–43. [ PubMed ] [ Google Scholar ]
- Considine, J. , Berry, D. , Doric, A. , Simpson, J. , Dwyer, A. , Hirth, S. , & Newnham, E. (in press). Frequency and nature of MET afferent limb failure in patients with documented vital sign abnormalities: A retrospective point prevalence study . Australian Critical Care . [ PubMed ] [ Google Scholar ]
- Considine, J. , & Currey, J. (2015). Ensuring a proactive, evidence‐based, patient safety approach to patient assessment . Journal of Clinical Nursing , 24 ( 1–2 ), 300–307. 10.1111/jocn.12641 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Considine, J. , Hutchison, A. F. , Rawson, H. , Hutchinson, A. , Bucknall, T. , Dunning, T. , Botti, M. , Duke, M. M. , & Street, M. (2018). Comparison of policies for recognising and responding to clinical deterioration across five Victorian health services . Australian Health Review , 42 ( 4 ), 412–419. 10.1071/AH16265 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cretikos, M. A. , Bellomo, R. , Hillman, K. , Chen, J. , Finfer, S. , & Flabouris, A. (2008). Respiratory rate: The neglected vital sign . Medical Journal of Australia , 188 , 657–659. [ PubMed ] [ Google Scholar ]
- Davies, O. , Devita, M. A. , Ayinla, R. , & Perez, X. (2014). Barriers to activation of the rapid response system . Resuscitation , 85 ( 11 ), 1557–1561. 10.1016/j.resuscitation.2014.07.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donohue, L. A. , & Endacott, R. (2010). Track, trigger and teamwork: Communication of deterioration in acute medical and surgical wards . Intensive and Critical Care Nursing , 26 ( 1 ), 10–17. 10.1016/j.iccn.2009.10.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Douw, G. , Schoonhoven, L. , Holwerda, T. , Huisman‐de Waal, G. , van Zanten, A. R. H. , Achterberg, T. , & van der Hoeven, J. G. (2015). Nurses' worry or concern and early recognition of deteriorating patients on general wards in acute care hospitals: A systematic review . Critical Care , 19 ( 1 ), 230. 10.1186/s13054-015-0950-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flabouris, A. , Chen, J. , Hillman, K. , Bellomo, R. , & Finfer, S. (2010). Timing and interventions of emergency teams during the MERIT study . Resuscitation , 81 ( 1 ), 25–30. [ PubMed ] [ Google Scholar ]
- Flabouris, A. , Nandal, S. , Vater, L. , Flabouris, K. , O'Connell, A. , & Thompson, C. (2015). Multi‐tiered observation and response charts: Prevalence and incidence of triggers, modifications and calls, to acutely deteriorating adult patients . PLoS One , 10 ( 12 ), e0145339. 10.1371/journal.pone.0145339 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guinane, J. , Bucknall, T. , Currey, J. , & Jones, D. (2013). Missed medical emergency team activations: Tracking decisions and outcomes in practice . Critical Care and Resuscitation , 15 ( 4 ), 266–272. [ PubMed ] [ Google Scholar ]
- Jones, D. , Baldwin, I. , McIntyre, T. , Story, D. , Mercer, I. , Miglic, A. , Goldsmith, D. , & Bellomo, R. (2006). Nurses' attitudes to a medical emergency team service in a teaching hospital . Quality and Safety in Health Care , 15 ( 6 ), 427–432. 10.1136/qshc.2005.016956 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jung, B. , Daurat, A. , De Jong, A. , Chanques, G. , Mahul, M. , Monnin, M. , Molinari, N. , & Jaber, S. (2016). Rapid response team and hospital mortality in hospitalized patients . Intensive Care Medicine , 42 ( 4 ), 494–504. 10.1007/s00134-016-4254-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Massey, D. , Chaboyer, W. , & Anderson, V. (2017). What factors influence ward nurses' recognition of and response to patient deterioration? An integrative review of the literature . Nursing Open , 4 ( 1 ), 6–23. 10.1002/nop2.53 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mok, W. Q. , Wang, W. , Cooper, S. , Ang, E. N. K. , & Liaw, S. Y. (2015). Attitudes towards vital signs monitoring in the detection of clinical deterioration: Scale development and survey of ward nurses . International Journal for Quality in Health Care , 27 ( 3 ), 207–213. 10.1093/intqhc/mzv019 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mok, W. Q. , Wang, W. , & Liaw, S. Y. (2015). Vital signs monitoring to detect patient deterioration: An integrative literature review . International Journal of Nursing Practice , 21 , 91–98. 10.1111/ijn.12329 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mullins, C. F. , & Psirides, A. (2016). Activities of a medical emergency team: A prospective observational study of 795 calls . Anaesthesia and Intensive Care , 44 ( 1 ), 34–43. 10.1177/0310057x1604400107 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Santiano, N. , Young, L. , Hillman, K. , Parr, M. , Jayasinghe, S. , Baramy, L.‐S. , Stevenson, J. , Heath, T. , Chan, C. , Claire, M. , & Hanger, G. (2009). Analysis of medical emergency team calls comparing subjective to “objective” call criteria . Resuscitation , 80 ( 1 ), 44–49. [ PubMed ] [ Google Scholar ]
- Shearer, B. , Marshall, S. , Buist, M. D. , Finnigan, M. , Kitto, S. , Hore, T. , Sturgess, T. , Wilson, S. , & Ramsay, W. (2012). What stops hospital clinical staff from following protocols? An analysis of the incidence and factors behind the failure of bedside clinical staff to activate the rapid response system in a multi‐campus Australian metropolitan healthcare service . BMJ Quality and Safety , 21 ( 7 ), 569–575. 10.1136/bmjqs-2011-000692 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Silva, R. , Saraiva, M. , Cardoso, T. , & Aragão, I. C. (2016). Medical emergency team: How do we play when we stay? Characterization of MET actions at the scene . Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine , 24 ( 1 ), 33. 10.1186/s13049-016-0222-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sprogis, S. K. , Currey, J. , Jones, D. , & Considine, J. (2021). Understanding the pre‐medical emergency team tier of a mature rapid response system: A content analysis of guidance documents . Australian Critical Care , 34 ( 5 ), 427–434. 10.1016/j.aucc.2020.12.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gotzsche, P. C. , & Vandenbroucke, J. P. (2007). The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies . Lancet , 370 ( 9596 ), 1453–1457. 10.1016/s0140-6736(07)61602-x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- White, K. , Scott, I. A. , Bernard, A. , McCulloch, K. , Vaux, A. , Joyce, C. , & Sullivan, C. M. (2016). Patient characteristics, interventions and outcomes of 1151 rapid response team activations in a tertiary hospital: A prospective study . Internal Medicine Journal , 46 ( 12 ), 1398–1406. 10.1111/imj.13248 [ PubMed ] [ CrossRef ] [ Google Scholar ]
Chapter 6: Knowledge Integration
Case Study 4: Older Adult Client (continued)
Vital sign measurements , 1050 hrs, september 7, 2018.
- Sitting BP: 160/94 mm Hg right arm
- Pulse: 72 bpm (radial), 2+, regular rhythm
1. Which findings are considered abnormal for this adult client? What medical terminology is used to define/label these findings?
- The blood pressure is elevated: hypertension (without diagnosis).
2. What factors might cause the blood pressure reading to be higher than normal in this adult client?
- Operator error
- Anxiety, stress, or pain
- Caffeine, smoking, or nicotine in the preceding 30 minutes
- Recently took adrenergic stimulants such as phenylephrine or pseudoephedrine
- Bladder and bowel discomfort
- Tight clothing on arm or forearm
- Noisy, cold room
- Taken immediately after activity
- Movement during the pressure reading
3. What are the healthcare provider’s next actions based on the findings of this older client?
- Retake the blood pressure to ensure accuracy
- Take blood pressure in the other arm
- ensure the room is quiet
- dim the lights
- allow the client to sit quietly for five minutes, without talking
- then take three measurements, a few minutes apart, with the automatic cuff (with an automatic cuff, the blood pressure documented is the average of the three readings).
After the healthcare provider followed the above procedures, the results were:
September 7, 2018
1058 hrs Sitting BP: 156/92 mm Hg right arm P 70 bpm (radial)
1100 hrs Sitting BP: 148/90 mm Hg left arm
Automatic Cuff
5 mins later (1105 hrs)
Sitting BP: 150/86 mm Hg right arm P 66 bpm
2 mins later (1107 hrs)
Sitting BP: 144/84 mm Hg right arm P 68 bpm
2 mins later (1109 hrs)
Sitting BP: 156/82 mm Hg right arm P 62 bpm
Vital Sign Record – Blank (pdf)
Vital Sign Measurement Across the Lifespan - 1st Canadian edition Copyright © 2018 by Ryerson University is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Vital signs and early warning scores.Canberra: ACT Health; 2011
Vital signs and early warning scores procedure.Canberra: ACT Health; 2018
Recognising and responding to acute deterioration. National Safety and Quality Health Care Standards, 2nd edn. Sydney: ACSQHC; 2017
Alexis O. Providing best practice in manual pulse measurement. Br J Nurs. 2010; 19:(4)228-234 https://doi.org/10.12968/bjon.2010.19.4.46784
Bleyer AJ, Vidya S, Russell GB, Jones CM, Sujata L, Daeihagh P, Hire D. Longitudinal analysis of one million vital signs in patients in an academic medical center. Resuscitation. 2011; 82:(11)1387-1392 https://doi.org/10.1016/j.resuscitation.2011.06.033
Bunkenborg G, Poulsen I, Samuelson K, Ladelund S, Akeson J. Bedside vital parameters that indicate early deterioration. Int J Health Care Qual Assur. 2019; 32:(1)262-272 https://doi.org/10.1108/IJHCQA-10-2017-0206
Burchill C, Anderson B, O'Connor PC. Exploration of nurse practices and attitudes related to postoperative vital signs. Medsurg Nurs. 2015; 24:(4)249-255
Cahill H, Jones A, Herkes R Introduction of a new observation chart and education programme is associated with higher rates of vital-sign ascertainment in hospital wards. BMJ Qual Saf. 2011; 20:(9)791-796 https://doi.org/10.1136/bmjqs.2010.045096
Casey G. Pulse oximetry—what are we really measuring?. Nurs N Z. 2011; 17:(3)24-29
Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir Med. 2013; 107:(6)789-799 https://doi.org/10.1016/j.rmed.2013.02.004
Chester JG, Rudolph JL. Vital signs in older patients: age-related changes. J Am Med Dir Assoc. 2011; 12:(5)337-343 https://doi.org/10.1016/j.jamda.2010.04.009
Churpek MM, Adhikari R, Edelson DP. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation. 2016; 102:1-5 https://doi.org/10.1016/j.resuscitation.2016.02.005
Churpek MM, Yuen TC, Winslow C, Robicsek AA, Meltzer DO, Gibbons RD, Edelson DP. Multicenter development and validation of a risk stratification tool for ward patients. Am J Respir Crit Care Med. 2014; 190:(6)649-655 https://doi.org/10.1164/rccm.201406-1022OC
Clifton DA, Clifton L, Sandu DM, Smith GB, Tarassenko L, Vollam SA, Watkinson PJ. ‘Errors’ and omissions in paper-based early warning scores: the association with changes in vital signs—a database analysis. BMJ Open. 2015; 5:(7) https://doi.org/10.1136/bmjopen-2014-007376
Clinical Excellence Commission. Between the flags: standard calling criteria. 2021. https://www.cec.health.nsw.gov.au/keep-patients-safe/deteriorating-patient-program/between-the-flags/standard-calling-criteria (accessed 19 August 2021)
Coogan N, Marra A, Lomonaco EA. Assessing accurate BP measurement. Nursing. 2015; 45:(4)16-18 https://doi.org/10.1097/01.NURSE.0000461838.55540.6e
Cooper S, Cant R, Sparkes L. Respiratory rate records: the repeated rate?. J Clin Nurs. 2014; 23:(9-10)1236-1238 https://doi.org/10.1111/jocn.12234
Cardona-Morrell M, Prgomet M, Lake R, Nicholson M, Harrison R, Long J, Westbrook J, Braithwaite J, Hillman K. Vital signs monitoring and nurse–patient interaction: a qualitative observational study of hospital practice. Int J Nurs Stud. 2016; 56:9-16 https://doi.org/10.1016/j.ijnurstu.2015.12.007
DeVita MA, Smith GB, Adam SK ‘Identifying the hospitalised patient in crisis’—a consensus conference on the afferent limb of Rapid Response Systems. Resuscitation. 2010; 81:(4)375-382 https://doi.org/10.1016/j.resuscitation.2009.12.008
Respiratory rate 6: the benefits of continuous monitoring. 2018. http://tinyurl.com/edmrp3zj (accessed 13 August 2021)
, 9th edn. In: Dougherty L, Lister S, West-Oram A (eds). Chichester: Wiley; 2015
Elliott M, Coventry A. Critical care: the eight vital signs of patient monitoring. Br J Nurs. 2012; 21:(10)621-625 https://doi.org/10.12968/bjon.2012.21.10.621
Fernandez M, Burns K, Calhoun B, George S, Martin B, Weaver C. Evaluation of a new pulse oximeter sensor. Am J Crit Care. 2007; 16:(2)146-152 https://doi.org/10.4037/ajcc2007.16.2.146
Grainger A. Principles of temperature monitoring. Nurs Stand. 2013; 27:(50)48-55 https://doi.org/10.7748/ns2013.08.27.50.48.e7242
Hands C, Reid E, Meredith P, Smith GB, Prytherch DR, Schmidt PE, Featherstone PI. Patterns in the recording of vital signs and early warning scores: compliance with a clinical escalation protocol. BMJ Qual Saf. 2013; 22:(9)719-726 https://doi.org/10.1136/bmjqs-2013-001954
Hill A, Kelly E, Horswill MS, Watson MO. The effects of awareness and count duration on adult respiratory rate measurements: an experimental study. J Clin Nurs. 2018; 27:(3-4)546-554 https://doi.org/10.1111/jocn.13861
Hogan J. Why don't nurses monitor the respiratory rates of patients?. Br J Nurs. 2006; 15:(9)489-492 https://doi.org/10.12968/bjon.2006.15.9.21087
Measuring body temperature using a tympanic thermometer. 2020. https://www.nursingtimes.net/clinical-archive/assessment-skills/measuring-body-temperature-using-a-tympanic-thermometer-2-14-09-2020/ (accessed 19 August 2021)
Jubran A. Pulse oximetry. Crit Care. 2015; 19:(1) https://doi.org/10.1186/s13054-015-0984-8
Kellet J. The assessment and interpretation of vital signs, 2nd edn. In: DeVita M, Hillman K, Bellomo R (eds). Switzerland: Springer; 2017
Kellett J, Kim A. Validation of an abbreviated Vitalpac™ Early Warning Score (ViEWS) in 75,419 consecutive admissions to a Canadian regional hospital. Resuscitation. 2012; 83:(3)297-302 https://doi.org/10.1016/j.resuscitation.2011.08.022
Kellett J, Sebat F. Make vital signs great again – A call for action. Eur J Intern Med. 2017; 45:13-19 https://doi.org/10.1016/j.ejim.2017.09.018
Respiratory rate 1: why accurate measurement and recording are crucial. 2018. http://tinyurl.com/9dhnhej2 (accessed 13 August 2021)
Principles of monitoring postoperative patients. 2013. http://tinyurl.com/5xmbstjc (accessed 13 August 2021)
Liu C, Zheng D, Griffiths C, Murray A. Comparison of repeatability of blood pressure measurements between oscillometric and auscultatory methods. Comput Cardiol. 2015; 42:1073-1076 https://doi.org/10.1109/CIC.2015.7411100
Ludikhuize J, Borgert M, Binnekade J, Subbe C, Dongelmans D, Goossens A. Standardized measurement of the Modified Early Warning Score results in enhanced implementation of a Rapid Response System: A quasi-experimental study. Resuscitation. 2014; 85:(5)676-682 https://doi.org/10.1016/j.resuscitation.2014.02.009
Ludikhuize J, Smorenburg SM, de Rooij SE, de Jonge E. Identification of deteriorating patients on general wards; measurement of vital parameters and potential effectiveness of the Modified Early Warning Score. J Crit Care. 2012; 27:(4)424.e7-424.e13 https://doi.org/10.1016/j.jcrc.2012.01.003
Malgaard R, Larsen P, Hakonsen S. Effectiveness of respiratory rate in determining clinical deterioration: a systematic review protocol. JBI Database Syst Rev Implement Reports. 2016; 14:(7)19-27 https://doi.org/10.11124/JBISRIR-2016-002973
Massey D, Aitken LM, Chaboyer W. The impact of a nurse led rapid response system on adverse, major adverse events and activation of the medical emergency team. Intensive Crit Care Nurs. 2015; 31:(2)83-90 https://doi.org/10.1016/j.iccn.2014.11.005
McGhee TL, Weaver P, Solo S, Hobbs M. Vital signs reassessment frequency recommendation. Nurs Manage. 2016; 47:(9)11-12 https://doi.org/10.1097/01.NUMA.0000491132.98848.22
Mirdamadi A, Etebari M. Comparison of manual versus automated blood pressure measurement in intensive care unit, coronary care unit, and emergency room. ARYA Atheroscler. 2017; 13:(1)29-34
Mok W, Wang W, Cooper S, Ang ENK, Liaw SY. Attitudes towards vital signs monitoring in the detection of clinical deterioration: scale development and survey of ward nurses. Int J Qual Health Care. 2015; 27:(3)207-213 https://doi.org/10.1093/intqhc/mzv019
National Institute for Clinical Excellence. Acutely ill patients in hospital. Recognition of and response to acute illness in adults in hospital. 2007. http://tinyurl.com/483wcjvc (accessed 13 August 2021)
Nielsen LG, Folkestad L, Brodersen JB, Brabrand M. Inter-observer agreement in measuring respiratory rate. PLoS One. 2015; 10:(6) https://doi.org/10.1371/journal.pone.0129493
Parkes R. Rate of respiration: the forgotten vital sign. Emerg Nurse. 2011; 19:(2)12-17 https://doi.org/10.7748/en2011.05.19.2.12.c8504
Patient Safety Surveillance Unit. From death we learn 2014. 2014. http://tinyurl.com/ys863dee (accessed 13 August 2021)
Philip K, Richardson R, Cohen M. Staff perceptions of respiratory rate measurement in a general hospital. Br J Nurs. 2013; 22:(10)570-574 https://doi.org/10.12968/bjon.2013.22.10.570
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005; 111:(5)697-716 https://doi.org/10.1161/01.CIR.0000154900.76284.F6
Pretto JJ, Roebuck T, Beckert L, Hamilton G. Clinical use of pulse oximetry: Official guidelines from the Thoracic Society of Australia and New Zealand. Respirology. 2014; 19:(1)38-46 https://doi.org/10.1111/resp.12204
Resuscitation Council UK. The ABCDE approach. 2021. https://www.resus.org.uk/library/abcde-approach (accessed 13 August 2021)
Rolfe S. The importance of respiratory rate monitoring. Br J Nurs. 2019; 28:(8)504-508 https://doi.org/10.12968/bjon.2019.28.8.504
Rylance J, Baker T, Mushi E, Mashaga D. Use of an early warning score and ability to walk predicts mortality in medical patients admitted to hospitals in Tanzania. Trans R Soc Trop Med Hyg. 2009; 103:(8)790-794 https://doi.org/10.1016/j.trstmh.2009.05.004
Shahbabu B, Dasgupta A, Sarkar K, Sahoo SK. Which is more accurate in measuring blood pressure? A digital or an aneroid sphygmanometer. J Clin Diagn Res. 2016; 10:(3)LC11-LC14 https://doi.org/10.7860/JCDR/2016/14351.7458
Smith JJ, Bland SA, Mullett S. Temperature—the forgotten vital sign. Accid Emerg Nurs. 2005; 13:(4)247-250 https://doi.org/10.1016/j.aaen.2005.08.002
Sund-Levander M, Grodzinsky E. Assessment of body temperature measurement options. Br J Nurs. 2013; 22:(16)942-950 https://doi.org/10.12968/bjon.2013.22.16.942
Tollefson J, Hillman E. Clinical psychomotor skills: assessment tools for nurses, 7th edn. Melbourne: Cengage; 2019
Vink P, Tulek Z, Gillis K, Jönsson AC, Buhagiar J, Waterhouse C, Poulsen I. Consciousness assessment: A questionnaire of current neuroscience nursing practice in Europe. J Clin Nurs. 2018; 27:(21-22)3913-3919 https://doi.org/10.1111/jocn.14614
Respiratory rate 5: using this vital sign to detect deterioration. 2018. http://tinyurl.com/avueersy (accessed 13 August 2021)
Williams P. deWit's fundamental concepts and skills for nursing, 5th edn. St Louis (MI): Elsevier; 2018
World Health Organization. Pulse oximetry training manual. http://tinyurl.com/3bpjn5b2 (accessed 13 August 2021)
Yeung MS, Lapinsky SE, Granton JT, Doran DM, Cafazzo JA. Examining nursing vital signs documentation workflow: barriers and opportunities in general internal medicine units. J Clin Nurs. 2012; 21:(7-8)975-982 https://doi.org/10.1111/j.1365-2702.2011.03937.x
The global elements of vital signs' assessment: a guide for clinical practice
Malcolm Elliott
Senior Lecturer, Monash Nursing and Midwifery, Monash University, Melbourne, Australia
View articles · Email Malcolm

The assessment of vital signs is critical for safe, high-quality care. Vital signs' data provide valuable insight into the patient's condition, including how they are responding to medical treatment and, importantly, whether the patient is deteriorating. Although abnormal vital signs have been associated with poor clinical outcomes, research has consistently found that vital signs' assessment is often neglected in clinical practice. Factors contributing to this include nurses' knowledge, clinical judgement, culture, tradition and workloads. To emphasise the importance of vital signs' assessment, global elements of vital signs' assessment are proposed. The elements reflect key principles underpinning vital signs' assessment and are informed by evidence-based literature.
Vital signs' assessment is a key component of safe, high-quality care and a fundamental nursing priority. Trends in vital sign data provide early warning of impending sepsis and respiratory failure, and can independently predict mortality ( Churpek et al, 2014 ; Nielsen et al, 2015 ). Furthermore, vital signs' data is important for medical emergency teams and early warning scores to function effectively, but only if there is adherence to vital sign monitoring protocols ( Hands et al, 2013 ).
Despite their clinical importance, research has consistently found that vital signs' assessment is often inaccurate, incomplete or falsified ( Ludikhuize et al, 2012 ; Philip et al, 2013 ; Cooper et al, 2014 ). The reasons for this are not clear, but nurses' knowledge, skills and clinical judgement, culture, tradition and ritual, along with laziness and workload have been identified as contributing factors ( Hogan, 2006 ; Yeung et al, 2012 ; Philip et al, 2013 ; Burchill et al, 2015 ; Cardona-Morrell et al, 2016 ). It has therefore been recommended that nurses need ongoing education to improve their attitudes towards vital sign monitoring ( Mok et al, 2015 ).
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
1.3 Vital Signs
Vital signs are typically obtained prior to performing a physical assessment. Vital signs include temperature recorded in Celsius or Fahrenheit, pulse, respiratory rate, blood pressure, and oxygen saturation using a pulse oximeter. See Figure 1.8 [1] for an image of a nurse obtaining vital signs. Obtaining vital signs may be delegated to unlicensed assistive personnel (UAP) for stable patients, depending on the state’s Nurse Practice Act, agency policy, and appropriate training. However, the nurse is always accountable for analyzing the vital signs and instituting appropriate follow-up for out-of-range findings. See Appendix A to review a checklist for obtaining vital signs.

The order of obtaining vital signs is based on the patient and their situation. Health care professionals often place the pulse oximeter probe on the patient while proceeding to obtain their pulse, respirations, blood pressure, and temperature. However, in some situations this order is modified based on the urgency of their condition. For example, if a person loses consciousness, the assessment begins with checking their carotid pulse to determine if cardiopulmonary resuscitation (CPR) is required. [2]
Temperature
Accurate temperature measurements provide information about a patient’s health status and guide clinical decisions. Methods of measuring body temperature vary based on the patient’s developmental age, cognitive functioning, level of consciousness, and health status, as well as agency policy. Common methods of temperature measurement include oral, tympanic, axillary, temporal, no touch, and rectal routes. It is important to document the route used to obtain a patient’s temperature because of normal variations in temperature in different locations of the body. Body temperature is typically measured and documented in health care agencies in degrees Celsius (ºC). [3]
Oral Temperature
Normal oral temperature is 35.8 – 37.3ºC (96.4 – 99.1ºF). An oral thermometer is shown in Figure 1.9. [4] The device has blue coloring, indicating it is an oral or axillary thermometer, as opposed to a rectal thermometer that has red coloring. Oral temperature is reliable when it is obtained close to the sublingual artery. [5]
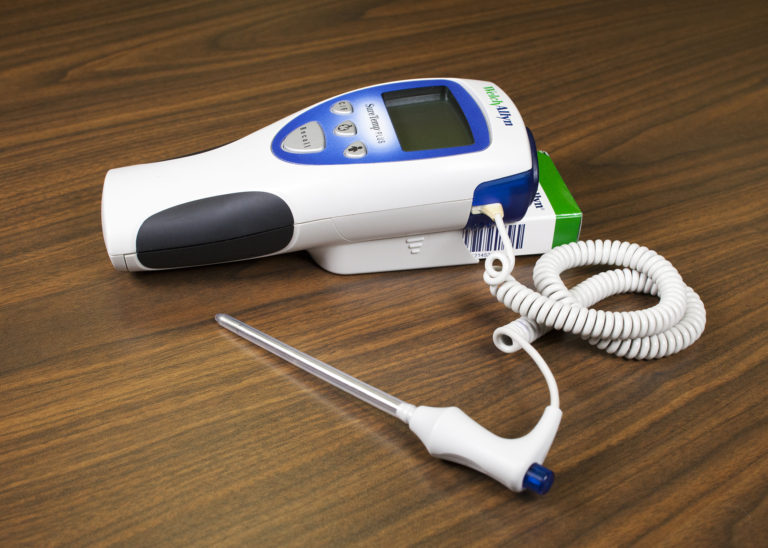
Remove the probe from the device and slide a probe cover (from the attached box) onto the oral thermometer without touching the probe cover with your hands. Place the thermometer in the posterior sublingual pocket under the tongue, slightly off-center. Instruct the patient to keep their mouth closed but not bite on the thermometer. Leave the thermometer in place for as long as is indicated by the device manufacturer. The thermometer typically beeps within a few seconds when the temperature has been taken. Read the digital display of the results. Discard the probe cover in the garbage (without touching the cover) and place the probe back into the device. [6] See Figure 1.10 [7] of an oral temperature being taken.

Some factors can cause an inaccurate measurement using the oral route. For example, if the patient recently consumed a hot or cold food or beverage, chewed gum, or smoked prior to measurement, a falsely elevated or decreased reading may be obtained. Oral temperature should be taken 15 to 25 minutes following consumption of a hot or cold beverage or food or 5 minutes after chewing gum or smoking. [8]
Tympanic Temperature
The tympanic temperature is typically 0.3 – 0.6°C or 0.5 – 1°F higher than an oral temperature. It is an accurate measurement because the tympanic membrane shares the same vascular artery that perfuses the hypothalamus (the part of the brain that regulates the body’s temperature). See Figure 1.11 [9] of a tympanic thermometer. The tympanic method should not be used if the patient has a suspected ear infection. [10] Accumulation of cerumen, earwax, may also reduce the accuracy of tympanic readings.

Remove the tympanic thermometer from its holder and place a probe cover on the thermometer tip without touching the probe cover with your hands. Turn the device on. Ask the patient to keep their head still. For an adult or older child, gently pull the helix (outer ear) up and back to visualize the ear canal. For an infant or child under age 3, gently pull the helix down. Insert the probe just inside the ear canal but never force the thermometer into the ear. The device will beep within a few seconds after the temperature is measured. Read the results displayed, discard the probe cover in the garbage (without touching the cover), and then place the device back into the holder. [11] See Figure 1.12 [12] for an image of a tympanic temperature being taken.

Axillary Temperature
The axillary method is a minimally invasive way to measure temperature and is commonly used in children. It uses the same electronic device as an oral thermometer (with blue coloring). However, the axillary temperature can be as much as 1ºC lower than the oral temperature. [13] An armpit (axillary) temperature is usually 0.3⁰ C (0.5⁰ F) to 0.6⁰ C (1⁰ F) lower than an oral temperature.
Remove the probe from the device and place a probe cover (from the attached box) on the thermometer without touching the cover with your hands. Ask the patient to raise their arm and place the thermometer probe in their armpit on bare skin as high up into the axilla as possible. The probe should be facing behind the patient. Ask the patient to lower their arm and leave the device in place until it beeps, usually about 10–20 seconds. Read the displayed results, discard the probe cover in the garbage (without touching the cover), and then place the probe back into the device. See Figure 1.13 [14] for an image of an axillary temperature. [15]

Rectal Temperature
Measuring rectal temperature is an invasive method. Some sources suggest its use only when other methods are not appropriate. However, when measuring infant temperature, it is considered a gold standard because of its accuracy. A rectal temperature is 0.5°F (0.3°C) to 1°F (0.6°C) higher than an oral temperature. [16] See Figure 1.14 [17] for an image of a rectal thermometer.
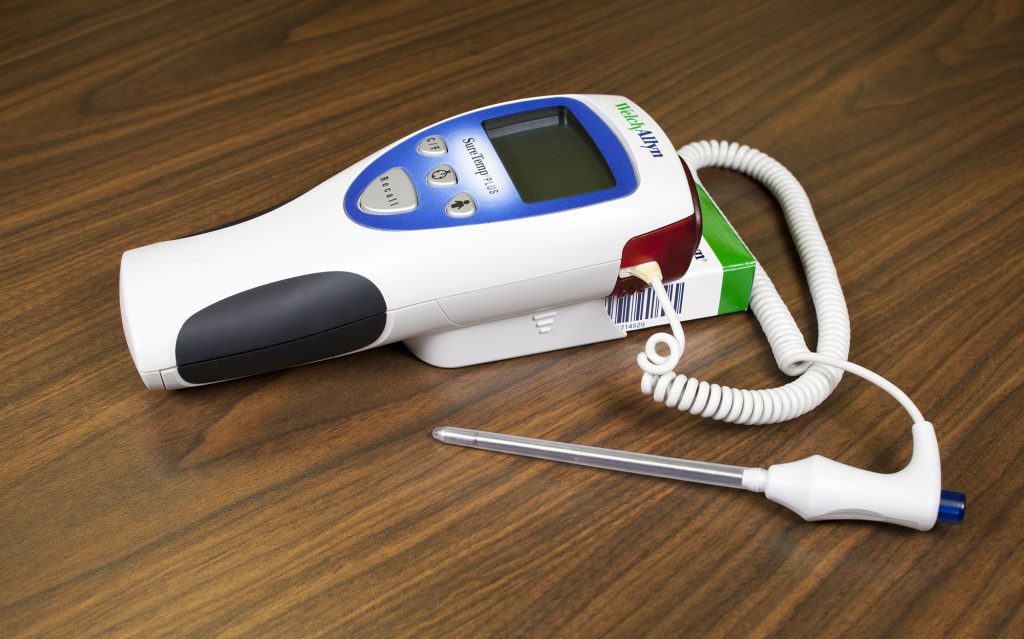
Before taking a rectal temperature, ensure the patient’s privacy. Wash your hands and put on gloves. For infants, place them in a supine position and raise their legs upwards toward their chest. Parents may be encouraged to hold the infant to decrease movement and provide a sense of safety. When taking a rectal temperature in older children and adults, assist them into a side lying position and explain the procedure. Remove the probe from the device and place a probe cover (from the attached box) on the thermometer. Lubricate the cover with a water-based lubricant, and then gently insert the probe 2–3 cm (approximately 0.5 in for babies less than 6 months old to 1 inch) into the anus or less, depending on the patient’s size. [18] Remove the probe when the device beeps. Read the result and then discard the probe cover in the trash can without touching it. Cleanse the device as indicated by agency policy. Remove gloves and perform hand hygiene.
Temporal Temperature
Temporal temperature is taken by using a device placed on the forehead. Temporal thermometers contain an infrared scanner that measures the heat on the surface of the skin resulting from blood moving through the temporal artery in the forehead. Temporal temperature is typically 0.5°F (0.3°C) to 1°F (0.6°C) lower than an oral temperature. It is a quick, noninvasive method, but accurate measurement is dependent on good contact with the skin and good placement on the forehead.
See Table 1.3a for normal temperature ranges for various routes.
Table 1.3 Normal Temperature Ranges [19]
| Oral | 35.8 – 37.3ºC (96.4 -99.1ºF) |
|---|---|
| Axillary | 34.8 – 36.3ºC (96.4 -97.3ºF) |
| Tympanic | 36.1 – 37.9ºC (97.0 -100.2ºF) |
| Rectal | 36.8 – 38.2ºC (98.2 -100.8ºF) |
| Temporal | 35.2 – 37.0ºC (95.4 – 98.6ºF) |
Pulse refers to the pressure wave that expands and recoils arteries when the left ventricle of the heart contracts. It is palpated at many points throughout the body. The most common locations to palpate pulses as part of vital sign measurement include radial, brachial, carotid, and apical areas as indicated in Figure 1.15. [20]
Pulse is measured in beats per minute wherever a pulse can be palpated. The normal adult pulse rate (heart rate) at rest is 60–100 beats per minute with different ranges according to age. The pulse rate is a measurement of the number of times the heart beats per minute. The pulse rate may differ from the heart rate if the force of the heart contraction is not strong enough to generate a pulse because the pulse is palpated whereas the heart rate is typically auscultated. See Table 1.3b for normal heart rate ranges by age. It is important to consider each patient situation when analyzing if their heart rate is within normal range. Begin by reviewing their documented baseline heart rate. Consider other factors if the pulse is elevated, such as the presence of pain or crying in an infant. It is best to complete the assessment when a patient is resting and comfortable, but if this is not feasible, document the circumstances surrounding the assessment and reassess as needed. [21] For example, pulse rate may be artificially elevated when individuals experience physical or mental stress. Therefore, it is best to collect a pulse rate assessment when the patient is resting.
Table 1.3b Normal Heart Rate by Age
| Preterm | 120 – 180 |
|---|---|
| Newborn (0 to 1 month) | 100 – 160 |
| Infant (1 to 12 months) | 80 – 140 |
| Toddler (1 to 3 years) | 80 – 130 |
| Preschool (3 to 5 years) | 80 – 110 |
| School Age (6 to 12 years) | 70 – 100 |
| Adolescents (13 to 18 years) and Adults | 60 – 100 |
Pulse Characteristics
When assessing pulses, the characteristics of rhythm, rate, force, and equality are included in the documentation.
Pulse Rhythm
A normal pulse has a regular rhythm, meaning the frequency of the pulsation felt by your fingers is an even tempo with equal intervals between pulsations. For example, if you compare the palpation of pulses to listening to music, it follows a constant beat at the same tempo that does not speed up or slow down. Some cardiovascular conditions, such as atrial fibrillation, cause an irregular heart rhythm. If a pulse has an irregular rhythm, document if it is “regularly irregular” (e.g., three regular beats are followed by one missed and this pattern is repeated) or if it is “irregularly irregular” (e.g., there is no rhythm to the irregularity). [22]
The pulse rate is counted with the first beat felt by your fingers as “One.” It is considered best practice to assess a patient’s pulse for a full 60 seconds, especially if there is an irregularity to the rhythm. [23]
Pulse Force
The pulse force is the strength of the pulsation felt on palpation. Pulse force can range from absent to bounding. The volume of blood, the heart’s functioning, and the arteries’ elastic properties affect a person’s pulse force. [24] Pulse force is documented using a four-point scale:
- 3+: Full, bounding
- 2+: Normal/strong
- 1+: Weak, diminished, thready
- 0: Absent/nonpalpable
If a pulse is absent, a Doppler ultrasound device is typically used to verify perfusion of the limbs. The Doppler is a handheld device that allows the examiner to hear the whooshing sound of the pulse. This device is also commonly used when assessing peripheral pulses in the lower extremities, such as the dorsalis pedis pulse or the posterior tibial pulse. See the following video demonstrating the use of a Doppler device.
View a YouTube Video of Using a Doppler Ultrasound Device to Assess a Pulse [25]
Pulse Equality
Pulse equality refers to a comparison of the pulse forces on both sides of the body. For example, a nurse often palpates the radial pulse on a patient’s right and left wrists at the same time and compares if the pulse forces are equal. However, the carotid pulses should never be palpated at the same time because this can decrease blood flow to the brain. Pulse equality provides data about medical conditions such as peripheral vascular disease and arterial obstruction. [26]
Radial Pulse
Use the pads of your first three fingers to gently palpate the radial pulse. The pads of the fingers are placed along the radius bone on the lateral side of the wrist (i.e., the thumb side). Fingertips are placed close to the flexor aspect of the wrist (i.e., where the wrist meets the hand and bends). See Figure 1.16 [27] for correct placement of fingers in obtaining a radial pulse. Press down with your fingers until you can feel the pulsation, but not so forcefully that you are obliterating the wave of the force passing through the artery. Note that radial pulses are difficult to palpate on newborns and children under the age of five, so the brachial or apical pulses are typically obtained in these populations. [28]

Carotid Pulse
The carotid pulse is typically palpated during medical emergencies because it is the last pulse to disappear when the heart is not pumping an adequate amount of blood. [29]
Locate the carotid artery medial to the sternomastoid muscle, between the muscle and the trachea, in the middle third of the neck. In order to palpate the carotid, place the index and middle fingers on the patient’s neck to the side of individual’s trachea. With the pads of your three fingers, gently palpate one carotid artery at a time so as not to compromise blood flow to the brain. See Figure 1.17 [30] for correct placement of fingers in a seated patient. [31]

Brachial Pulse
A brachial pulse is typically assessed in infants and children because it can be difficult to feel the radial pulse in these populations. If needed, a Doppler ultrasound device can be used to obtain the pulse.
The brachial pulse is located by feeling the bicep tendon in the area of the antecubital fossa. Move the pads of your three fingers medially from the tendon about 1 inch (2 cm) just above the antecubital fossa. It can be helpful to hyperextend the patient’s arm to accentuate the brachial pulse so that you can better feel it. You may need to move your fingers around slightly to locate the best place to accurately feel the pulse. You typically need to press fairly firmly to palpate the brachial pulse. [32] See Figure 1.18 [33] for correct placement of fingers along the brachial artery.

Apical Pulse
The apical pulse rate is considered the most accurate pulse and is indicated when obtaining assessments prior to administering cardiac medications. It is obtained by listening with a stethoscope over a specific position on the patient’s chest wall. Read more about listening to the apical pulse and other heart sounds in the “ Cardiovascular Assessment ” section.
Respiratory Rate
Respiration refers to a person’s breathing and the movement of air into and out of the lungs. Inspiration refers to the process causing air to enter the lungs, and expiration refers to the process causing air to leave the lungs. A respiratory cycle (i.e., one breath while measuring respiratory rate) is one sequence of inspiration and expiration. [34]
When obtaining a respiratory rate, the respirations are also assessed for quality, rhythm, and rate. The quality of a person’s breathing is normally relaxed and silent. However, loud breathing, nasal flaring, or the use of accessory muscles in the neck, chest, or intercostal spaces indicate respiratory distress. People experiencing respiratory distress also often move into a tripod position, meaning they are leaning forward and placing their arms or elbows on their knees or on a bedside table. If a patient is demonstrating new signs of respiratory distress as you are obtaining their vital signs, it is vital to immediately notify the health care provider or follow agency protocol.
Respirations normally have a regular rhythm in children and adults who are awake. A regular rhythm means that the frequency of the respiration follows an even tempo with equal intervals between each respiration. However, newborns and infants commonly exhibit an irregular respiratory rhythm.
Normal respiratory rates vary based on age. The normal resting respiratory rate for adults is 10–20 breaths per minute, whereas infants younger than one year old normally have a respiratory rate of 30–60 breaths per minute. See Table 1.3c for ranges of normal respiratory rates by age. It is also important to consider factors such as sleep cycle, presence of pain, and crying when assessing a patient’s respiratory rate. [35]
Read more about assessing a patient’s respiratory status in the “ Respiratory Assessment ” section.
Table 1.3c Normal Respiratory Rate by Age [36]
| Newborn to one month | 30 – 60 |
|---|---|
| One month to one year | 26 – 60 |
| 1-10 years of age | 14 – 50 |
| 11-18 years of age | 12 – 22 |
| Adult (ages 18 and older) | 10 – 20 |
Oxygen Saturation
A patient’s oxygenation status is routinely assessed using pulse oximetry, referred to as SpO2. SpO2 is an estimated oxygenation level based on the saturation of hemoglobin measured by a pulse oximeter. Because the majority of oxygen carried in the blood is attached to hemoglobin within the red blood cells, SpO2 estimates how much hemoglobin is “saturated” with oxygen. The target range of SpO2 for an adult is 94-100%. For patients with chronic respiratory conditions, such as chronic obstructive pulmonary disease (COPD), the target range for SpO2 is often lower at 88% to 92%. Although SpO2 is an efficient, noninvasive method to assess a patient’s oxygenation status, it is an estimate and not always accurate. For example, if a patient is severely anemic and has a decreased level of hemoglobin in the blood, the SpO2 reading is affected. Decreased peripheral circulation can also cause a misleading low SpO2 level.
A pulse oximeter includes a sensor that measures light absorption of hemoglobin. See Figure 1.19 [37] for an image of a pulse oximeter. The sensor can be attached to the patient using a variety of devices. For intermittent measurement of oxygen saturation, a spring-loaded clip is attached to a patient’s finger or toe. However, this clip is too large for use on newborns and young children; therefore, for this population, the sensor is typically taped to a finger or toe. An earlobe clip is another alternative for patients who cannot tolerate the finger or toe clip or have a condition, such as vasoconstriction or poor peripheral perfusion, that could affect the results.
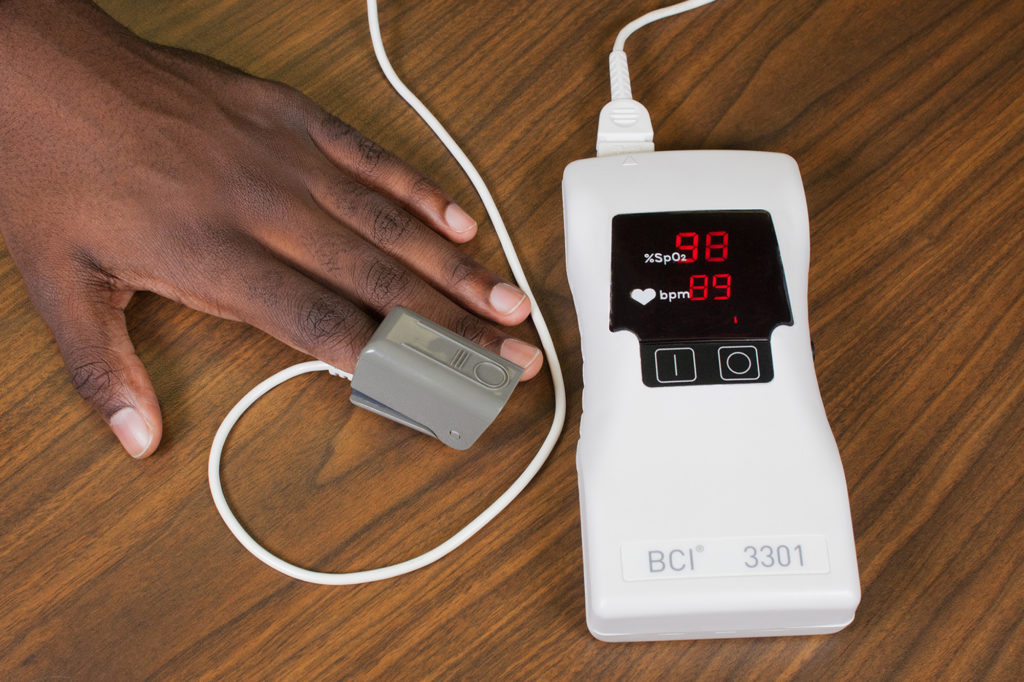
Read more about pulse oximetry in the “ Oxygen Therapy ” chapter.
Nail polish or artificial nails can affect the absorption of light waves from the pulse oximeter and decrease the accuracy of the SpO2 measurement when using a probe clipped on the finger. An alternative sensor that does not use the finger should be used for these patients or the nail polish should be removed. If a patient’s hands or feet are cold, it is helpful to clip the sensor to the earlobe or tape it to the forehead.
Blood Pressure
Read information about how to accurately obtain blood pressure measurement in the “ Blood Pressure ” chapter.
Interpreting Results
After obtaining a patient’s vital signs, it is important to immediately analyze the results, recognize deviations from expected normal ranges, and report deviations appropriately. As a nursing student, it is vital to immediately notify your instructor and/or collaborating nurse caring for the patient of any vital sign measurement out of normal range.
- “ US Navy 110714-N-RM525-060 Hospitalman Seckisiesha Isaac, from New York, prepares to take a woman's temperature at a pre-screening vital signs stat.jpg ” by U.S. Navy photo by Mass Communication Specialist 2nd Class Jonathen E. Davis is licensed under CC0 ↵
- Vital Sign Measurement Across the Lifespan by Ryerson University is licensed under CC BY-SA 4.0 ↵
- “Thermometer-oral-768x548.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.17%3A_Oral_Temperature ↵
- “Oral-Temperature-Wide-768x512.jpg" by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.17%3A_Oral_Temperature ↵
- “Tympanic-Thermometer.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.18%3A_Tympanic_Temperature ↵
- “Tympanic-Temperature-Correct-2.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.18%3A_Tympanic_Temperature ↵
- “Axilla-Temperature-1-768x596.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.19%3A_Axillary_Temperature ↵
- “Thermometer-rectal-768x479.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/02%3A_Temperature/2.20%3A_Rectal_Temperature ↵
- “Radial-brachial-carotid-and-apical-pulse-final-930x1024.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.15%3A_What_is_Pulse%3F ↵
- Ryerson University. (2018, March 21). Doppler device - How to [Video]. YouTube. All rights reserved. https://youtu.be/cn3aA0G1mgc ↵
- “Radial-pulse-correct.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.18%3A_Radial_Pulse ↵
- “Carotid-pulse-768x511.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.19%3A_Carotid_Pulse ↵
- “Brachial-pulse.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/03%3A_Pulse_and_Respiration/3.20%3A_Brachial_Pulse ↵
- “02-Sat-Apparatus-1-1-1024x682.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Vital_Sign_Measurement_Across_the_Lifespan_(Lapum_et_al.)/04%3A_Oxygen_Saturation/4.09%3A_How_is_Oxygen_Saturation_Measured%3F ↵
Nursing Skills - 2e Copyright © 2023 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
15.3 Vital Signs
Learning objectives.
By the end of this section, you will be able to:
- Describe the steps involved for preparing to obtain vital signs
- Understand how and when to monitor vital signs
- Discuss the importance of using critical judgment when validating data
- Explain proper techniques for documenting data
A vital sign is a marker of physiological homeostasis and are essential in the analysis of monitoring patient progress. Vital signs include the body temperature, pulse, respiratory rate, and blood pressure. Vital signs are gathered during the initial encounter with the patient to establish a baseline and routinely thereafter, according to condition, to assess disease progression or resolution. When vital signs are abnormal, a patient’s plan of care is typically altered. When vital signs are taken routinely, the healthcare team can analyze them to observe the response to treatments or disease progression. The combination of multiple vital sign measurements over a period of time also provides the typical and normal ranges for an individual patient. These individualized ranges are the vital sign trends. The vital signs provide a snapshot of the circulatory, respiratory, and neurological status of the patient.
Preparing to Obtain Vital Signs
Prior to obtaining vital signs, the nurse should gather the necessary equipment, check the patient’s vital sign trends and pertinent history, and verify the healthcare provider’s orders regarding frequency and parameters. To complete the vital signs, the nurse must obtain a thermometer, stopwatch, stethoscope, pulse oximeter, and blood pressure cuff. Many of these items may be present on the facility’s vital sign machine. Some facilities keep designated vital sign equipment at the patient’s bedside. At times, vital signs are obtained via an electronic monitoring device either continually (such as in critical care units) or scheduled ( Figure 15.14 ). When these devices are used, it is the nurse’s responsibility to manually collect the data received.
Reviewing the patient’s vital sign trends could provide valuable information for the nurse. For example, if the patient’s health record indicates that their heart rate is typically around 65 beats per minute, then the nurse checks it and finds it to be 96 beats per minute, further investigation may be warranted. Although this value is normal for the population in general, it is not normal for that patient.
Health history may influence obtaining vital signs. For example, a mastectomy would prevent the nurse from obtaining blood pressure on that arm due to the risk of lymphedema , and a wound might prevent placement of blood pressure cuff. Oral trauma would change the route of obtaining the temperature, and a wound over the wrist may interfere with the palpation of a pulse . Being prepared prior to entering the room will prevent errors.
Life-Stage Context
Older adults and normal temperature ranges.
The normal temperature range in older adults tends to be on the lower end of the normal adult temperature ranges. As we age, our metabolic rate gradually decreases which, in turn, causes a gradual decline in our temperature. When caring for an older adult, a temperature on the high end of normal could indicate a fever, and even a serious infection, since their trends are lower (Hernandes Júnior & Sardeli, 2021).
Monitoring Vital Signs
The frequency at which a nurse should obtain vital signs is determined by the stability of the patient, facility protocols, and healthcare provider orders. Heart rate, respiratory rate, blood pressure, and oxygen saturation may be monitored continuously in critical settings or with patients who are unable to manage their airways or sufficiently perfuse their body. It is important to note that the nurse can use nursing judgment to recheck vital signs at any time despite the frequency noted in the orders. The orders indicate the minimum frequency by which the nurse should take the patient’s vital signs. Any change in the patient’s status such as a new complaint or new assessment finding would prompt the nurse to obtain a set of vital signs. Whenever a nurse feels that the practitioner needs to be updated on the patient’s status, the nurse should obtain a complete set of vital signs to communicate a thorough picture of the patient to the practitioner.
Clinical Judgment Measurement Model
Take action: change in patient status.
A nurse is caring for a gentleman recovering from a total knee replacement, postoperative day 2. The healthcare provider has ordered vital signs every four hours, physical therapy, pain medications, and a resumption of home medications. Since surgery, he has been doing well in physical therapy, and his pain has been controlled with IV ketorolac (Toradol) and oral acetaminophen (Tylenol). He last received ketorolac at 0430. His last set of vital signs were obtained two hours ago at 0400:
- Temperature 98.1°F (36.7°C)
- Pulse 68 beats per minute
- Respiratory rate 16 breaths per minute
- Blood pressure 119/58 mm Hg
This morning, he stated that his pain has been getting worse, not better, since his last dose of pain medicine. He also asked for Tylenol for a headache.
After noting the change in the patient’s condition, the nurse needs to take action. Even though it is not time to obtain the ordered vital signs, nursing judgment dictates the need to get another set of them. The vital signs are as follows:
- Temperature 99.8°F (37.7°C)
- Pulse 84 beats per minute
- Respiratory rate 22 breaths per minute
- Blood pressure 132/64 mm Hg
After administering the dose of acetaminophen, the nurse contacts the healthcare provider to report the change in the patient’s condition and the updated vital signs.
Postoperatively, vital signs are monitored according to a facility’s protocol, with more frequent vital signs obtained initially after the procedure, which then is progressively spaced out to the unit protocol frequency ( Table 15.4 ). This postoperative protocol is used because of the anesthesia and medication’s effects and the nature of the procedure. Anesthesia and medication may cause respiratory depression and other reactions, among other complications. The procedure itself could have caused bleeding or damage to a body area. More frequently measured vital sign s may show subtle changes, which can then be used to determine the healthcare team’s course of action.
| Protocol | Time | Data |
|---|---|---|
| Immediately | 1015 | |
| Every fifteen minutes for the first hour | 1030 1045 1100 1115 | |
| Every thirty minutes for two hours | 1145 1215 1245 1315 | |
| Every hour for four hours | 1415 1515 1615 1715 | |
| Revert to unit protocol’s or healthcare practitioner’s orders |
Consider this scenario: A patient has arrived from the operating room after an emergency appendectomy. The unit postoperative vital sign protocol is as follows: Obtain vital signs on arrival to the unit, then every fifteen minutes × one hour, every thirty minutes × two hours, every hour × four hours, every four hours throughout admission. Following is an example of why vital sign monitoring is so important in discovering subtle changes and performing interventions to prevent complications.
| Time | Data | Observations/Interventions |
|---|---|---|
| 1015 | HR 67, BP 108/62, O 98, RR 14 | Patient sleepy; arrived to unit |
| 1030 | HR 72, BP 112/68, O 98, RR 18 | Wife at bedside |
| 1045 | HR 82, BP 120/74, O 98, RR 20 | Patient reporting pain; pain meds given |
| 1100 | HR 64, BP 102/58, O 94, RR 12 | Patient resting with lower O and RR; order obtained for 2 L O via nasal cannula |
| 1115 | HR 66, BP 108/62, O 95, RR 14 | Patient resting comfortably |
| 1145 | HR 76, BP 112/68, O 95, RR 16 | Patient reporting pain; nonpharmacological interventions done |
| 1215 | HR 72, BP 110/68, O 95, RR 16 | Patient resting comfortably |
| 1245 | HR 70, BP 108/64, O 92, RR 14 | Patient encouraged to use incentive spirometer/cough and deep breathe |
| 1315 | HR 76, BP 112/64, O 92, RR 12 | Practitioner made aware of O saturation; nasal cannula increased to 4 L O |
| 1415 | HR 74, BP 110/62, O 94, RR 14 | Reinforced the importance of incentive spirometer use; raised the head of the bed for better lung expansion |
| 1515 | HR 78, BP 112/62, O 96, RR 16 | Encouraged continuation of incentive spirometer use; nasal cannula decreased to 2 L O |
| 1615 | HR 76, BP 107/62, O 96, RR 16 | Encouraged continuation of incentive spirometer use |
| 1715 | HR 78, BP 110/68, O 97, RR 16 | Encouraged continuation of incentive spirometer use |
Through vital sign monitoring, the nurse was able to identify possible postoperative atelectasis (partial collapse of the lung from anesthesia) and begin interventions to halt progress into possible pneumonia .
Different settings and their protocols may also affect the frequency of the vital signs. In intensive care units, which are those units where the patients are in critical condition, even more frequent assessment may be necessary depending on patient condition and medications. In long-term care settings, vital signs are obtained every eight to twelve hours. In home health environments or when individuals are instructed to monitor their vital signs at home, they are typically done once each day and at the same time each day. Doing them at the same time each day helps the individual to make monitoring vital signs a habit. Another reason to do them at the same time each day is to prevent fluctuations due to the individual’s normal routine and time of day. Heart rate would be expected to be lower first thing in the morning and higher as the day progresses.
If there is a change in a patient’s condition, the nurse must obtain another set of vital signs, even if the last set was obtained only one hour prior. Changes in the patient’s condition refer to something experienced by the patient or observed by the nurse or family members—that is, anything that is concerning to any of the parties. The checked vital signs can help to alleviate the patient’s or family’s fears, but they may also provide the data that need to be conveyed to the healthcare provider to determine the next actions.
Validating Data
After the nurse obtains vital signs, it is imperative to compare these against the normal ranges for the patient’s age and the patient’s trends. Generally, if the results fall within both ranges, the vital signs are documented according to protocol. If the results fall outside of the normal ranges or the patient’s trends, the nurse will need to validate them, that is, to repeat the measurement of the vital sign in question. At times, these abnormal results reflect the clinical situation of the patient, but at other times, the abnormalities may be a result of operator or equipment error.
When an abnormal vital sign is obtained, whether outside of the normal ranges or outside of the patient’s trends, the nurse should recheck that vital sign. If the temperature reading is abnormal, the nurse may try another thermometer or use another route. Changing equipment will allow the nurse to ensure that the abnormal reading was not caused by equipment malfunction. If the equipment malfunction is noted, the nurse should report it, take the equipment out of use, notify biomed/tech to check the equipment, and label the equipment as “do not use.”
The nurse may also just have to verify that the steps were completed accurately in obtaining the temperature. For an abnormal blood pressure reading, it may be necessary to recheck on the opposite arm. Automatic and digital vital sign equipment has preset limits for results it is able to provide. For example, some digital thermometers will give an error screen if the result is greater than 105°F (40.5°C). If a patient’s results are outside of these limits, a manual method for obtaining that vital sign will be necessary. Any abnormal results warrant a reassessment of that vital sign. The nurse must also assess the patient for any signs of distress or deterioration. There are times when abnormal results do not indicate an emergency or need for intervention. Vital signs may be abnormally high when the patient is excited, nervous, or has experienced physical activity, such as physical therapy. They also may be lower due to the comforting presence of family or friends.
Documenting Data
After vital signs are obtained and validated, the nurse must document these results. Most healthcare facilities use the electronic health record for patients, but some facilities still use paper flowsheets. Documentation is required to track the patient’s trends and response to treatments and to communicate with the healthcare team. For temperature, the nurse will chart the degrees in Fahrenheit or Celsius (according to agency policy) and the method used to obtain the temperature (i.e., oral, axilla, tympanic). When charting the pulse, the result will be in beats per minute. The nurse will also document the site or method used for the pulse (i.e., radial pulse or continuous pulse oximeter). The respiratory rate will be documented in breaths per minute, and the method of assessment should be noted (i.e., visual or stethoscope). Blood pressure requires two numbers to be documented, the systolic and the diastolic pressures. The nurse will also specify which extremity was used and if the blood pressure was manually or automatically obtained. For an abnormal result, whether the charting system flags the vital sign or not, the action should be documented. For example, the action may be that a medication was administered, that the patient’s position was changed, or that the healthcare provider was alerted.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/clinical-nursing-skills/pages/1-introduction
- Authors: Christy Bowen
- Publisher/website: OpenStax
- Book title: Clinical Nursing Skills
- Publication date: Jun 26, 2024
- Location: Houston, Texas
- Book URL: https://openstax.org/books/clinical-nursing-skills/pages/1-introduction
- Section URL: https://openstax.org/books/clinical-nursing-skills/pages/15-3-vital-signs
© Jun 12, 2024 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
85 Case Study 1: Adult Client (continued)
1. What infection control measures should the healthcare provider implement? Use correct handwashing techniques before and after your assessment.
2. What method should be used to measure temperature for this adult client? Temperature is best taken using the tympanic or axillary route; because the client is nauseated, the oral route could stimulate the gag reflex.
3. What pulse and blood pressure readings should be taken for this adult client? Orthostatic vital signs (pulse and blood pressure) should be taken because this client is at risk for hypovolemia. The client may be dehydrated as a result of the vomiting and diarrhea and lack of fluid intake. Return to the chapter on blood pressure for more information on hypovolemia and its effects on vital signs.
Next, see and read the vital sign record below. On a piece of paper, write down each of the client’s vital sign readings, and if applicable, the route used and the client’s position.
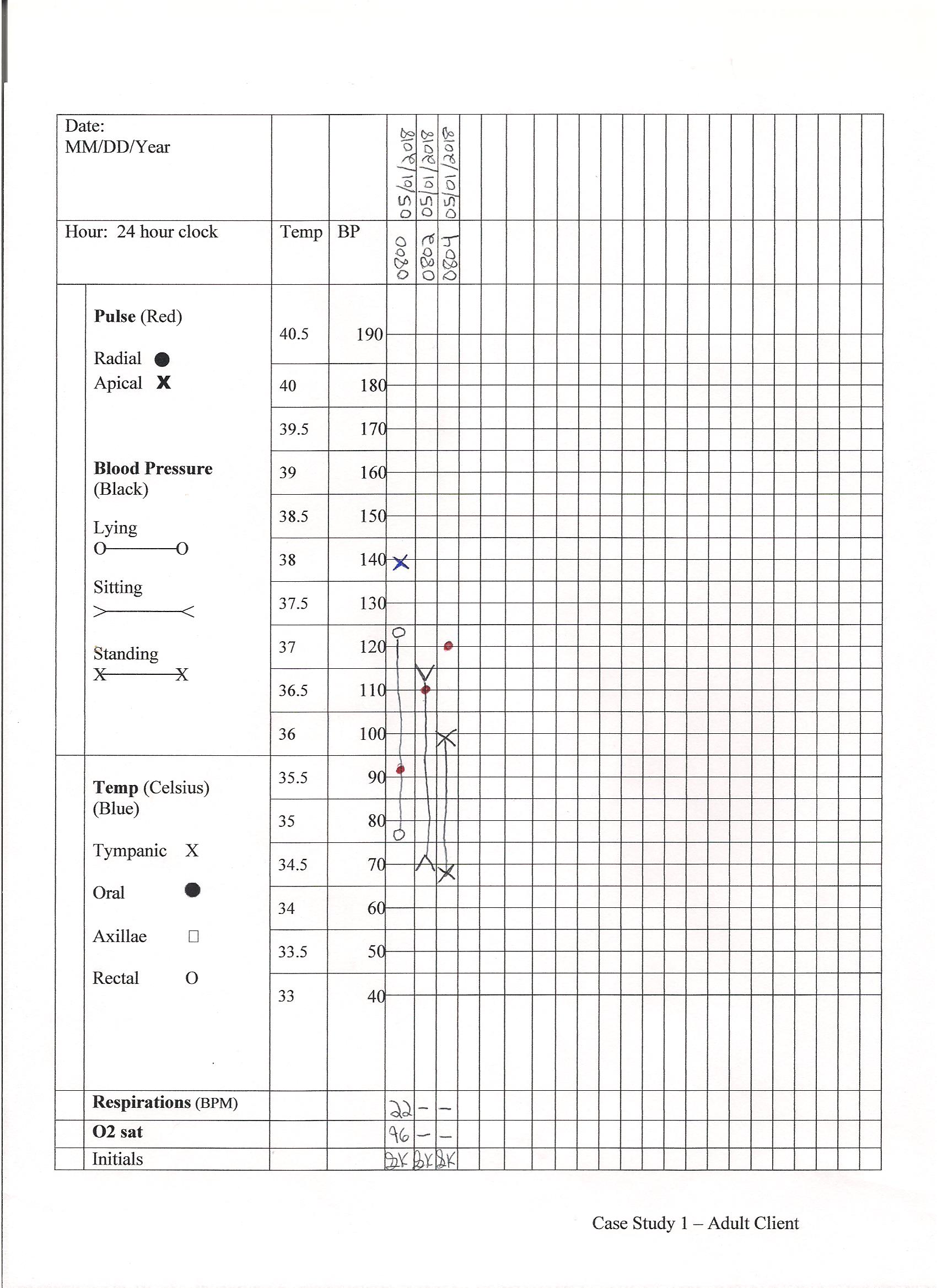
Vital Sign Measurement Across the Lifespan - 1st Canadian edition Copyright © 2018 by Ryerson University is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.
Volume 27, Number 5—May 2021
Epidemiologic Findings from Case Investigations and Contact Tracing for First 200 Cases of Coronavirus Disease, Santa Clara County, California, USA
Author affiliations: Centers for Disease Control and Prevention, Atlanta, Georgia, USA (N. Ortiz, J.T. Lee, K.L. Bajema, J.N. Ricaldi, M. Cortese, A.E. Barskey, J.F. Da Silva, M. Fischer, S.J. Chai) ; County of Santa Clara Public Health Department, San Jose, California, USA (E. Villarino, S. Smith, W. Lin, B.J. Bonin, S.L. Rudman, G.S. Han, S.H. Cody)
Cite This Article
In January 2020, Santa Clara County, California, USA, began identifying laboratory-confirmed coronavirus disease among residents. County staff conducted case and contact investigations focused on households and collected detailed case demographic, occupation, exposure, and outcome information. We describe the first 200 test-positive cases during January 31–March 20, 2020, to inform future case and contact investigations. Probable infection sources included community transmission (104 cases), known close contact with a confirmed case-patient (66 cases), and travel (30 cases). Disease patterns across race and ethnicity, occupational, and household factors suggested multiple infection risk factors. Disproportionately high percentages of case-patients from racial and ethnic subgroups worked outside the home (Hispanic [86%] and Filipino [100%]); household transmission was more common among persons from Vietnam (53%). Even with the few initial cases, detailed case and contact investigations of household contacts capturing occupational and disaggregated race and ethnicity data helped identify at-risk groups and focused solutions for disease control.
On January 31, 2020, the Santa Clara County Department of Public Health (SCCDPH) in San Jose, California, USA, identified its first case of coronavirus disease (COVID-19) in a resident who had recently returned from Wuhan, China ( 1 ). On February 28, the county reported its first case of COVID-19 associated with probable community transmission, 48 hours after the first presumed community-acquired case in the United States was identified 91 miles north in Solano County ( 2 ). Staff of the SCCDPH, the California Department of Public Health, and the Centers for Disease Control and Prevention (CDC) began conducting detailed interviews with each case-patient or their surrogate to identify, quarantine, and monitor close contacts, and isolate and test those who were symptomatic. Santa Clara initiated a series of community mitigation strategies to slow the spread of the virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), including canceling large gatherings ( 3 , 4 ). On March 16, Santa Clara and 5 adjacent San Francisco Bay Area counties became the first US region to implement shelter-in-place orders requiring all residents to limit activity outside of their home and to order nonessential businesses and operations to close ( 5 ). SCCPHD collected detailed information on demographic characteristics to help identify communities at risk and those disproportionately affected by COVID-19. Since the initial identification of cases, surges in COVID-19 incidence have often constrained public health and community capacity to respond, including overwhelming case and contact investigation efforts. We describe the epidemiology of the first 200 COVID-19 cases reported to SCCPHD to identify key transmission factors that could already be identified early in the COVID-19 pandemic through detailed case investigation and contact tracing focused on households and to demonstrate the utility of focusing these efforts throughout the pandemic response.
Case Identification and Testing
We defined a confirmed COVID-19 case as an illness in a resident of Santa Clara County with SARS-CoV-2 detected by reverse transcription PCR (RT-PCR) on a nasopharyngeal or oropharyngeal swab specimen by a public health, hospital, or reference clinical microbiology laboratory or CDC. Testing was recommended in line with the following evolving CDC Person Under Investigation case definition: clinical findings of lower respiratory illness and travel to a Wuhan, China (later expanded to all of China) or an epidemiologic link to a laboratory-confirmed COVID-19 case ( 6 , 7 ); hospitalization for severe respiratory disease and no alternative diagnosis ( 8 ); and clinically compatible illness regardless of travel or known contact with a confirmed case-patient. Included COVID-19 case-patients comprised those reported to SCCDPH and those identified by a community-based sentinel surveillance project for COVID-19 conducted during March 5–14, 2020, among clinic patients with respiratory illness who tested negative for influenza virus ( 9 ). This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.
Case Investigation and Contact Tracing
SCCDPH, California Department of Public Health, and CDC staff identified cases reported to California’s electronic reportable disease system. Staff interviewed COVID-19 cases or their surrogates for information on case age, sex, race, ethnicity, address, occupation, travel history, known contact with another confirmed case-patient, symptom onset (earliest of any symptoms listed on CDC’s standardized case report form) ( 10 ), and hospitalization. Investigators collected detailed race and ethnicity data, including racial subgroup among case-patients reporting Asian ancestry.
Case-patients with no recent travel and no known close contact with another confirmed case-patient in the 2 weeks before symptom onset were classified as probable community transmission. Known close contact was defined as living with, caring for, working with, transporting, or prolonged exposure (close contact <6 feet for > 30 minutes) to a person with confirmed COVID-19. Case-patients with any travel outside of Santa Clara County in the 2 weeks before their symptom onset were considered travel-associated cases.
SCCPHD’s contact tracing involved identifying persons with close contact with the case-patient 2 weeks after the case-patient’s symptom onset and notifying contacts of their exposure. Owing to the rapid rise in case counts and limited personnel capacity, the team focused on following up with household contacts. In-hospital outcomes were collected from review of medical records and case-patient interviews. Deaths through May 20, 2020 (60 days after the 200th case was reported), were defined as COVID-19–associated if the cause or other contributing cause on the death certificate was listed as COVID-19.
Data Analysis
We collected data using standard forms and open-ended case-patient interviews and entered results into Excel 365 (Microsoft, https://www.microsoft.com ) and California’s electronic reportable disease system. Categorical variables were described as counts and percentages, and continuous variables were described using median and range. We estimated associations between illness severity measures (hospitalization defined as admission for > 1 night in an inpatient acute-care facility [including intensive-care unit (ICU) stay and mechanical intubation with ventilation]; ICU stay [including mechanical ventilation]; mechanical ventilation; and death) as the dependent variables, and age and sex as independent variables with odds ratios (ORs) and 95% CIs using bivariate logistic regression. Because of the limited number of cases, to avoid invalid results or unstable models, measurements were not adjusted. We analyzed data using Stata 14 (StataCorp, https://www.stata.com ) and Epi Info version 7 (Epi Info, https://www.cdc.gov/epiinfo ) and generated maps using Excel 365 (Microsoft, https://www.microsoft.com ).
Case Description
- Figure 1 . Week of symptom onset, for first 200 confirmed coronavirus disease cases, by exposure source, Santa Clara County, California, USA, January 31–March 20, 2020.
Of the 200 cases with laboratory confirmation of SAR-CoV-2 positivity during January 31–March 20, 2020, a total of 191 (96%) were identified through routine surveillance and contact tracing and 9 (4%) were identified through clinic-based sentinel surveillance. Onset of illness ranged from January 24 through March 18; these case-patients were exposed before shelter-in-place orders were invoked ( Figure 1 ). Among the first cases identified during January 31–February 2, travel accounted for the largest reported source of exposure. Over subsequent weeks, case-patients reported unknown and household exposure at higher frequencies than other exposures. The percentage of case-patients who were hospitalized decreased over time as testing availability increased and focus of testing broadened to include additional populations, including symptomatic contacts.

Figure 2 . Hospitalization status and outcomes, for first 200 confirmed coronavirus disease cases, by age group, Santa Clara County, California, USA, January 31–March 20, 2020. Outcomes are classified by most severe status...
Among the 200 case-patients, 112 (56%) were male, and the median age was 50 years (range 6 months–94 years); only 10 (5%) case-patients were <20 years of age, whereas 71 (36%) were > 60 years of age ( Table ). The racial and ethnic distribution of case-patients was similar to that of the county population overall: 70 (35%) reported as Asian, 52 (26%) Hispanic, 52 (26%) White non-Hispanic, 4 (2%) Black non-Hispanic, and 3 (1%) Pacific Islander; race or ethnicity was unknown for 19 (9%) case-patients. Although Asian-identifying persons comprised a similar proportion of case-patients as that of Santa Clara County, a higher proportion of case-patients identified as Filipino (10% vs. 5%), a similar proportion as Vietnamese (7% vs. 7%), and a lower proportion as Indian (4% vs. 9%) or Chinese (4% vs. 10%) than among the general population of Santa Clara County ( 11 , 12 ). Of the 200 case-patients, 89 (44%) were hospitalized ( Table ); 45 (23%) were on a general ward, 18 (9%) were admitted to an ICU without requiring mechanical ventilation, and 26 (13%) required mechanical ventilation in an ICU. The proportion of case-patients hospitalized, admitted to the ICU, requiring mechanical ventilation, and who died each increased with increasing age ( Figure 2 ). Compared with case-patients <60 years of age, case-patients > 60 years of age had higher odds of hospitalization (OR 4.4 [95% CI 2.4–8.3]), ICU stay (OR 10.9 [95% CI 4.9–24.2]), mechanical ventilation (OR 6.3 [95% CI 2.5–16.0]), and death (OR 9.0 [95% CI 2.9–28.4]). No statistically significant association was observed between clinical outcomes and sex.
Among the 200 case-patients, 20 (10%) had a matching death certificate. The median age of deceased case-patients was 70.5 years (range 42–87 years), and 15 (75%) were male. Among the 20 case-patients who died, 9 (45%) were Asian, 5 (25%) were White non-Hispanic, 2 (10%) were Hispanic, and 4 (20%) had unknown race or ethnicity. Five (25%) of the 20 deaths occurred among persons of Filipino ethnicity; these case-patients did not have a known close contact to one another.

Figure 3 . Geographic location of first 200 confirmed coronavirus disease cases, by case-patient’s ZIP code area of residence (for those areas with >2,000 residents), Santa Clara County, California, USA, January 31–March 20,...
Case-patient residences were distributed among 47 (79%) of the 59 ZIP codes in the county; 18 (30%) ZIP codes had 1–2 cases, 13 (22%) had 3–4 cases, and 16 (8%) had > 5 cases ( Figure 3 , panel A). Case-patient residences clustered in the northeastern part of the county, where 2 adjacent ZIP codes accounted for 36 (18%) of the 200 case-patients; in the ZIP code with the most cases, 9 were associated with a single household. COVID-19 incidence rates by ZIP code ranged from 0–113 cases/100,000 persons; rates were generally highest in eastern ZIP codes in the county ( Figure 3 , panel B).
Exposure Type and Setting
Of the 200 case-patients, 66 (33%) had known close contact with another confirmed case-patient, 30 (15%) were considered travel-associated cases ( Table ), and 104 (52%) were attributable to probable community transmission. Among the 66 case-patients with known close contact with another confirmed case-patient, 49 (74%) were exposed to a household member, and 17 (26%) had occupational exposures. Most households with evidence of transmission (13/15 [86%]) had 2–3 confirmed case-patients identified. However, 2 multigenerational households each had 9 and 4 case-patients; the cluster of 4 case-patients was only identified as a result of contact tracing.
Of the 200 case-patients, 159 (79%) were adults with reported occupation. Of these, 111 (69%) were actively employed (not retired and reported employment), and of these, 82 (73%) reported jobs requiring work outside the home, which included healthcare workers, firefighters, food service workers, retail employees, construction workers, housekeepers, and other workers. Among these 82 case-patients reporting jobs requiring work outside the home, 46% of exposures were attributable to probable community transmission, followed by 22% household and 21% occupational exposures.
Type and location of exposure, as well as having an occupation that requires work outside the home, varied by race and ethnicity. Among 49 cases in Hispanic adults, occupation was known for 44 (89%); of the 38 actively employed, 89% held occupations that required them to work outside of the home. Occupation was known for 16 of 20 Filipino case-patients; for the 9 case-patients who were actively employed, all had jobs outside the home. Occupational exposure to a confirmed case-patient, including in a healthcare setting, accounted for 5 (25%) of 20 cases in Filipino persons, compared with 12 (7%) of all other cases with reported race and ethnicity. Household transmission accounted for exposures in 53% of Vietnamese case-patients and 32% of Hispanic case-patients, compared with 23% of all other case-patients with known race/ethnicity. Among case-patients of Indian and Chinese ethnicity, >50% had travel-related exposures.
Among the 17 case-patients with an occupational exposure to a confirmed case-patient, 11 (64%) exposures occurred in a nonhealthcare setting. Of these 11, all were employed as essential workers in occupations or settings in which they had frequent contact with many persons in the community. Occupational clusters and groupings included 6 airport employees, 4 employees at a supermarket, 3 childcare workers who shared a classroom and bathroom, and 2 firefighters who worked at the same station. At least 3 additional cases were identified among other firefighters who worked at the same station or attended a common function but were not Santa Clara County residents.
Of the 200 case-patients, 16 (8%) were healthcare workers with jobs that provided direct patient care or were first responders with direct patient exposure, of whom 8 (50%) were nurses. Only 6 transported, cared for, or had other known close contact with a confirmed case-patient in a healthcare setting. Of the other 10 cases in healthcare workers, 1 case-patient had travel-related exposure, 3 had known close contact with a case-patient in their household, and 6 did not have exposure to a known COVID-19 case-patient and were categorized as attributable to probable community transmission.
Detailed case investigations and household contact tracing of the first 200 case-patients of COVID-19 in Santa Clara County were able to help elucidate factors associated with being a COVID-19 case-patient and identify populations at risk for infection early in the response, including possible racial and ethnic disparities, elevated risks within households, and high-risk occupational groups. Many of these factors and populations at risk were subsequently confirmed by studies later in the pandemic ( 13 , 14 ). Case investigations identified possible sources of transmission in 96 (48%) of cases, and for those case-patients with known exposure, household transmission was the most commonly reported source, especially in Vietnamese and Hispanic communities. Work outside the home was commonly reported by Hispanic case-patients. Case-patients > 60 years of age had significantly higher odds of being hospitalized, being admitted to the ICU, requiring mechanical ventilation, and dying; these findings are consistent with reports from China, Italy, and other parts of the United States ( 15 – 17 ).
Because SCCPHD conducted contact tracing and monitoring specifically among household contacts of case-patients, the finding that approximately one quarter of the first 200 case-patients were household contacts of a confirmed case-patient is not surprising. However, SCCPHD’s prioritization of contact tracing and monitoring contacts within households early in the pandemic was high-yield, and findings were consistent with disease transmission factors for COVID-19 reported in subsequent studies ( 18 , 19 ). Investigations identified not only that older persons had increased odds of poor outcomes from COVID-19 but also that case-patients with multiple factors potentially increased risk. For example, several large clusters were identified within families that consisted of members of multiple generations, and several individuals >80 years of age might have been exposed. In 2 of these clusters, the index case-patient was a nonelderly household member who presumably transmitted SARS-CoV-2 to elderly household members. Anecdotally, several of these households also reported crowding and inability to self-isolate from other members within the home (Santa Clara COVID-19 Case Investigation Team, pers. comm., group discussion during case review, March 2020). Households have been identified as a high-risk setting for SARS-CoV-2 transmission ( 20 – 22 ), and household crowding is a risk factor for COVID-19 ( 23 ). In the ZIP code with the highest case rate in northeast Santa Clara, 14% of households are overcrowded (>1.0 persons/room), as measured by the American Community Survey, compared with the median of 6% of households in Santa Clara County as a whole ( 24 ). Although information on an individual case-patient’s household density was not collected as part of case and contact investigations, 4 (33%) of 12 ZIP codes where household transmission was identified reported >10% frequency of overcrowded households, compared with 7 (20%) of 35 ZIP codes where cases were identified but no household transmission was noted. Household density might be associated with other factors, such as high-risk occupations of household members ( 25 , 26 ), to increased risk for COVID-19 within households. Case investigators collecting information regarding household density during interviews can help not only to elucidate transmission risk in a particular household, but also link persons at high risk for poor outcomes to resources to prevent household transmission. One example of a solution to prevent household transmission is The NYC Test and Trace Corps, a collaborative public health program led by NYC Health + Hospitals in collaboration with the New York City Department of Public Health and Mental Hygiene, which offers hotel stays for persons who have COVID-19, exhibit COVID-19 symptoms, or are contacts of a known COVID-19 case-patient and who need to isolate or quarantine from household members ( 27 ).
Working outside the home, especially with public-facing duties (e.g., airport workers), was especially common in this early cohort; >40% of case-patients reported an occupation that did not allow them to work from home. A large frequency of case-patients who performed work outside the home did not report a known exposure or travel, suggesting that difficult-to-trace exposures, such as exposure to someone the case-patient did not know or did not know was infected, probably occurred ( 28 ). Moreover, occupational exposures were probably more common than we reported, because case-patients who did not have known exposure to a person with confirmed COVID-19 and had not traveled were classified as having community exposure. Identifying the source of exposure for case-patients with occupations that interact with the public might prove to be very labor-intensive or impossible, given the number of potential contacts involved. However, case and contact investigations, at a minimum, should include notifying co-workers and alerting employers to a positive case in a workplace ( 29 ) and collecting occupation data to help identify occupational subgroups at risk.
Occupational exposures probably differed by racial and ethnic groups among the first 200 case-patients in Santa Clara County. Among employed Filipino case-patients, all held jobs that required work outside the home. Although few Hispanic case-patients reported an occupational exposure with a confirmed COVID-19 case-patient, a greater percentage of Hispanic case-patients (89%) had occupations that required them to work outside the home than did White non-Hispanic case-patients (56%). Many of the Hispanic case-patients in Santa Clara County communicated that they could not afford the lost wages that would result from staying home from work (Santa Clara COVID-19 Case Investigation Team, pers. comm., group discussion during case review, March 2020). Hispanic persons nationwide have reported higher frequencies of job loss and wage reduction because of the COVID-19 pandemic compared with persons from other racial and ethnic minority groups, and less than one third of Hispanic persons surveyed reported that they could weather a financial emergency ( 30 ). These financial and occupational factors together might be critical drivers for transmission within the Hispanic population in Santa Clara County and perhaps statewide, where Hispanic persons have accounted for a disproportionately high number of cases ( 31 ). A disproportionately high percentage of COVID-19 cases and deaths occurred in Filipino persons; cases among Filipino persons associated with occupational exposures involved providing direct patient care to known COVID-19 patients or contact with a person with confirmed COVID-19 in public-facing service jobs.
Household exposures also differed by racial and ethnic groups. Vietnamese and Hispanic case-patients more frequently reported exposure to a person with confirmed COVID-19 in their household compared with case-patients from other race and ethnicity groups. Anecdotally, among Vietnamese and Hispanic case-patients, > 3 reported living in multigenerational households with high densities of persons and an inability to self-isolate within the home, posing a serious risk to older adults residing in these households. Household case clusters occurred in eastern ZIP codes that had high percentages of Hispanic persons (58% of the population in the ZIP code with the most cases and highest rates) and Vietnamese persons (22%), compared with 26% of Hispanic and 7% of Vietnamese persons in the county as a whole ( 32 – 37 ). Together, these findings suggest that household crowding might be an especially important driver of household transmission in traditionally underserved communities.
Few of the first 200 COVID-19 cases in Santa Clara County occurred in healthcare workers or persons in institutional or congregate living settings. Although more than one third of infected healthcare workers reported an occupational exposure and a quarter traveled or had a nonoccupational close-contact exposure, none of these exposures was identified for 40% of them. Evidence to date does not support substantial occupational transmission of SARS-CoV-2 to healthcare workers ( 38 ). Community transmission could have been an important source of exposure for healthcare workers, given the widespread community transmission occurring simultaneously in Santa Clara County.
One limitation of this analysis is, as with most reports on COVID-19, case identification was largely dictated by testing practices. At the start of the outbreak, the number of persons eligible for testing according to CDC criteria and testing capacity were limited, biasing these initial findings to case-patients with higher disease and mortality rates and to persons with recent travel or known contact with a confirmed case-patient. Had testing been more widely available and criteria included milder symptoms or risk for exposure regardless of symptoms, broader or earlier detection of community transmission might have occurred. This investigation occurred when information was limited for this new and emerging disease. The definition of prolonged COVID-19 exposure and guidance for case and contact investigations has been updated since this investigation concluded ( 39 ). Although we observed differences in sources of exposure by race and ethnicity, data on race were missing for 19 (9%) cases and racial subgroup for 16 (23%) of 70 cases among Asian persons; therefore, these data should be interpreted with caution. Our data reflect the epidemiology of COVID-19 in Santa Clara early in the pandemic among those with clinical manifestations that were eligible for testing and probably are not reflective of the current epidemiology ( 40 ).
Even with results from only the first 200 case-patients, detailed case investigation and contact tracing focused on households revealed patterns of at-risk populations, including older age adults, racial and ethnic subgroups, occupational categories, and potentially crowded households. Detailed case reviews, including disaggregation of race and ethnicity data, helped identify local factors of transmission and disparities important for public health intervention. Importantly, occupational exposures continue to be a source of infection ( 41 ), and understanding transmission risk within specific occupational settings, especially among professions that require persons to work outside their homes, is important to ensure safe workplaces and reopening of economies as the pandemic continues to evolve. As mitigation measures to suppress community transmission evolve throughout the pandemic response, novel preventive measures (e.g., temporary housing) might continue to be necessary to protect disproportionately affected subpopulations and older adults.
Dr. Ortiz is an Epidemic Intelligence Service Officer in the Division of Scientific Education and Professional Development, Center For Surveillance, Epidemiology, And Laboratory Services, Centers for Disease Control and Prevention.
Members of the Santa Clara County COVID-19 Case Investigation Team: Nora Chea, Calin Chiribau, Lindsey Duca, Joseph Hicks, Jimee Hwang, Jessica Leung, Joel London, Huong Pham, Matthew Stuckey, Diya Surie, Kathleen Thurman, and Douglas Trout.
Acknowledgment
We thank the Case Investigation Team for their support in the field.
- Santa Clara County Public Health Department . Letter from the Health Officer. February 3, 2020 [ cited 2021 Jan 28 ]. https://www.sccgov.org/sites/covid19/Pages/health-officer-letter-2-3-2020.aspx
- Santa Clara County Public Health Department . County of Santa Clara Public Health Department reports third case of COVID-19. February 28, 2020 [ cited 2021 Jan 28 ]. https://www.sccgov.org/sites/phd/news/Pages/third-novel-coronavirus-case-02-2020.aspx
- Santa Clara County Public Health Department . County of Santa Clara issues order to cancel mass gatherings due to increasing rates of COVID-19. March 9, 2020 [ cited 2021 Jan 28 ]. https://www.sccgov.org/sites/phd/news/Pages/order-health-officer-03092020.aspx
- Santa Clara County Public Health Department . Due to increasing rates of COVID-19, County Public Health issues new order cancelling gatherings of more than 100 people and restricting gatherings of more than 35 people. March 13, 2020 [ cited 2021 Jan 28 ]. https://www.sccgov.org/sites/phd/news/Pages/press-release-03-13-20.aspx .
- Santa Clara County Public Health Department . Seven bay area jurisdictions order residents to stay home. March 16, 2020 [ cited 2021 Jan 28 ]. https://www.sccgov.org/sites/phd/news/Pages/press-release-03-16-20.aspx
- Centers for Disease Control and Prevention . Health alert network: update and interim guidance on outbreak of 2019 novel coronavirus ( 2019 -nCOV) in Wuhan, China. 2020 [ cited 2021 Jan 28 ]. https://emergency.cdc.gov/han/han00427.asp
- Centers for Disease Control and Prevention . Health alert network: update and interim guidance on outbreak of 2019 novel coronavirus ( 2019 -nCOV) in Wuhan, China. 2020 [ cited 2021 Jan 28 ]. https://emergency.cdc.gov/han/han00426.asp
- Centers for Disease Control and Prevention . Update and interim guidance on outbreak of coronavirus disease 2019 (COVID-19). February 28, 2020 [ cited 2021 Jan 28 ]. https://emergency.cdc.gov/han/2020/han00428.asp
- Zwald ML , Lin W , Sondermeyer Cooksey GL , Weiss C , Suarez A , Fischer M , et al. Rapid sentinel surveillance for COVID-19—Santa Clara County, California, March 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 419 – 21 . DOI PubMed Google Scholar
- Centers for Disease Control and Prevention . Human infection with 2019 novel coronavirus case report form [ cited 2021 Jan 29 ]. https://www.cdc.gov/coronavirus/2019-ncov/downloads/pui-form.pdf
- US Census Bureau . United States Census. Quick facts: Santa Clara County, California. July 1, 2019 [ cited 2021 Jan 28 ]. https://www.census.gov/quickfacts/santaclaracountycalifornia
- US Census Bureau . 2018 American Community Survey 5-year estimates, demographic and housing estimates, Table DP05 [ cited 2021 Jan 28 ]. https://data.census.gov/cedsci/table?g=0400000US06_0500000US06085&d=ACS%205-Year%20Estimates%20Data%20Profiles&tid=ACSDP5Y2018.DP05
- Figueroa JF , Wadhera RK , Lee D , Yeh RW , Sommers BD . Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood) . 2020 ; 39 : 1984 – 92 . DOI PubMed Google Scholar
- Grijalva CG , Rolfes MA , Zhu Y , McLean HQ , Hanson KE , Belongia EA , et al. Transmission of SARS-COV-2 infections in households—Tennessee and Wisconsin, April–September 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 1631 – 4 . DOI PubMed Google Scholar
- Grasselli G , Zangrillo A , Zanella A , Antonelli M , Cabrini L , Castelli A , et al. ; COVID-19 Lombardy ICU Network . Baseline characteristics and outcomes of 1591 cases infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA . 2020 ; 323 : 1574 – 81 . DOI PubMed Google Scholar
- Garg S , Kim L , Whitaker M , O’Halloran A , Cummings C , Holstein R , et al. Hospitalization rates and characteristics of cases hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 458 – 64 . DOI PubMed Google Scholar
- Bialek S , Boundy E , Bowen V , Chow N , Cohn A , Dowling N , et al. ; CDC COVID-19 Response Team . Severe outcomes among cases with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 343 – 6 . DOI PubMed Google Scholar
- Qian G , Yang N , Ma AHY , Wang L , Li G , Chen X , et al. COVID-19 transmission within a family cluster by presymptomatic carriers in China. Clin Infect Dis . 2020 ; 71 : 861 – 2 . DOI PubMed Google Scholar
- Chan JF-W , Yuan S , Kok K-H , To KK , Chu H , Yang J , et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet . 2020 ; 395 : 514 – 23 . DOI PubMed Google Scholar
- Wang Z , Ma W , Zheng X , Wu G , Zhang R . Household transmission of SARS-CoV-2. J Infect . 2020 ; 81 : 179 – 82 . DOI PubMed Google Scholar
- Haroon S , Chandan JS , Middleton J , Cheng KK . Covid-19: breaking the chain of household transmission. BMJ . 2020 ; 370 : m3181 . DOI PubMed Google Scholar
- Lei H , Xu X , Xiao S , Wu X , Shu Y . Household transmission of COVID-19-a systematic review and meta-analysis. J Infect . 2020 ; 81 : 979 – 97 . DOI PubMed Google Scholar
- Emeruwa UN , Ona S , Shaman JL , Turitz A , Wright JD , Gyamfi-Bannerman C , et al. Associations between built environment, neighborhood socioeconomic status, and SARS-CoV-2 infections among pregnant women in New York City. JAMA . 2020 ; 324 : 390 – 2 . DOI PubMed Google Scholar
- US Census Bureau . Percentage of overcrowded housing units, 2014–2018 American Community Survey 5-year estimates. Table B25014 [ cited 2021 Jan 30 ]. https://data.census.gov/cedsci/table?q=B25014&tid=ACSDT5Y2018.B25014&hidePreview=false
- Ghinai I , Woods S , Ritger KA , McPherson TD , Black SR , Sparrow L , et al. Community transmission of SARS-CoV-2 at two family gatherings—Chicago, Illinois, February–March 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 446 – 50 . DOI PubMed Google Scholar
- Centers for Disease Control and Prevention . Households living in close quarters. April 18, 2020 [ cited 2021 Jan 29 ]. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/living-in-close-quarters.html
- Test & Trace Corps . NYC Health + Health Hospitals. Take care [ cited 2021 Jan 29 ]. https://www.nychealthandhospitals.org/test-and-trace/take-care
- US Department of Labor, Occupational Safety and Health Administration . Safety and Health Topics. COVID-19. Hazard recognition [ cited 2020 Jul 13 ]. https://www.osha.gov/coronavirus/hazards
- Council of State and Territorial Epidemiologists Occupational Health Subcommittee . Recommended interim guidance for collecting employment information about COVID-19 cases [ cited 2021 Jan 28 ]. https://cdn.ymaws.com/www.cste.org/resource/resmgr/publications/Guidance_collecting_io_covid.pdf
- Pew Research Center . About half of lower-income Americans report household job or wage loss due to COVID-19. April 21, 2020 [ cited 2021 Jan 28 ]. https://www.pewsocialtrends.org/2020/04/21/about-half-of-lower-income-americans-report-household-job-or-wage-loss-due-to-covid-19
- California Department of Public Health . COVID-19 race and ethnicity data. June 7, 2020 [ cited 2021 Jan 28 ]. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Race-Ethnicity.aspx
- Census Reporter . 95127. ZIP code tabulation area in: Santa Clara County, CA, San Jose-Sunnyvale-Santa Clara, CA Metro Area, California, United States [ cited 2021 Jan 28 ]. https://censusreporter.org/profiles/86000US95127-95127
- Census Reporter . 95148. ZIP code tabulation area in: Santa Clara County, CA, San Jose-Sunnyvale-Santa Clara, CA Metro Area, California, United States [ cited 2021 Jan 28 ]. https://censusreporter.org/profiles/86000US95148-95148
- Census Reporter. Santa Clara County. CA [ cited 2021 Jan 28 ]. https://censusreporter.org/profiles/05000US06085-santa-clara-county-ca
- Census Reporter . Race. American Community Survey 2018 5-year estimates. Table B02001 [ cited 2021 Jan 28 ]. https://censusreporter.org/data/table/?table=B02001&geo_ids=86000US95148&primary_geo_id=86000US95148#valueType|estimate
- US Census Bureau . Asian alone by selected groups. American Community Survey 2018 5-year estimates. Table B02015 [ cited 2021 Jan 28 ]. https://data.census.gov/cedsci/table?q=B02015&g=8600000US95148&tid=ACSDT5Y2018.B02015&hidePreview=false
- US Census Bureau . Hispanic or Latino origin by specific origin. American Community Survey 2018 5-year estimates. Table B03001 [ cited 2021 Jan 29 ]. https://data.census.gov/cedsci/table?q=Table%20B03001&tid=ACSDT5Y2018.B03001&hidePreview=false
- Kambhampati AK , O’Halloran AC , Whitaker M , Magill SS , Chea N , Chai SJ , et al. ; COVID-NET Surveillance Team . COVID-19-associated hospitalizations among health care personnel—COVID-NET, 13 states, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 1576 – 83 . DOI PubMed Google Scholar
- Centers for Disease Control and Prevention . Investigating a COVID-19 case [ cited 2021 Jan 29 ]. https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/investigating-covid-19-case.html
- Santa Clara County Public Health. County of Santa Clara Emergency Operations Center COVID-19 dashboards [ cited 2021 Jan 29 ]. https://www.sccgov.org/sites/covid19/Pages/dashboard-demographics-of-cases-and-deaths.aspx
- Fisher KA , Olson SM , Tenforde MW , Feldstein LR , Lindsell CJ , Shapiro NI , et al. ; IVY Network Investigators ; CDC COVID-19 Response Team . CDC COVID-19 Response Team. Telework before illness onset among symptomatic adults aged > 18 years with and without COVID-19 in 11 outpatient health care facilities—United States, July 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 1648 – 53 . DOI PubMed Google Scholar
- Figure 2 . Hospitalization status and outcomes, for first 200 confirmed coronavirus disease cases, by age group, Santa Clara County, California, USA, January 31–March 20, 2020. Outcomes are classified by most severe...
- Figure 3 . Geographic location of first 200 confirmed coronavirus disease cases, by case-patient’s ZIP code area of residence (for those areas with >2,000 residents), Santa Clara County, California, USA, January 31–March...
- Table . Characteristics of first 200 confirmed COVID-19 case-patients, Santa Clara County, California, USA, January 31–March 20, 2020
DOI: 10.3201/eid2705.204876
Original Publication Date: April 01, 2021
1 Members of the Santa Clara County COVID-19 Case Investigation Team are listed at the end of this article.
Table of Contents – Volume 27, Number 5—May 2021
| EID Search Options |
|---|
| – Search articles by author and/or keyword. |
| – Search articles by the topic country. |
| – Search articles by article type and issue. |
Please use the form below to submit correspondence to the authors or contact them at the following address:
Nancy Ortiz, Centers for Disease Control and Prevention, 1600 Clifton Rd NE, Mailstop V25-1, Atlanta, GA 30329-4027, USA
Comment submitted successfully, thank you for your feedback.
There was an unexpected error. Message not sent.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Article Citations
Highlight and copy the desired format.
| EID | Ortiz N, Villarino E, Lee JT, Bajema KL, Ricaldi JN, Smith S, et al. Epidemiologic Findings from Case Investigations and Contact Tracing for First 200 Cases of Coronavirus Disease, Santa Clara County, California, USA. Emerg Infect Dis. 2021;27(5):1301-1308. https://doi.org/10.3201/eid2705.204876 |
|---|---|
| AMA | Ortiz N, Villarino E, Lee JT, et al. Epidemiologic Findings from Case Investigations and Contact Tracing for First 200 Cases of Coronavirus Disease, Santa Clara County, California, USA. . 2021;27(5):1301-1308. doi:10.3201/eid2705.204876. |
| APA | Ortiz, N., Villarino, E., Lee, J. T., Bajema, K. L., Ricaldi, J. N., Smith, S....Cody, S. H. (2021). Epidemiologic Findings from Case Investigations and Contact Tracing for First 200 Cases of Coronavirus Disease, Santa Clara County, California, USA. , (5), 1301-1308. https://doi.org/10.3201/eid2705.204876. |
Metric Details
Article views: 2316.
Data is collected weekly and does not include downloads and attachments. View data is from .
What is the Altmetric Attention Score?
The Altmetric Attention Score for a research output provides an indicator of the amount of attention that it has received. The score is derived from an automated algorithm, and represents a weighted count of the amount of attention Altmetric picked up for a research output.

IMAGES
VIDEO
COMMENTS
Case Study 1: Adult Client (continued) 1. What infection control measures should the healthcare provider implement? ... Orthostatic vital signs (pulse and blood pressure) should be taken because this client is at risk for hypovolemia. The client may be dehydrated as a result of the vomiting and diarrhea and lack of fluid intake. Return to the ...
Case Studies, Chapter: Vital Signs. You are a nurse caring for a 58-year-old ironworker who has been admitted to your unit with acute hypertension. He became extremely symptomatic at work and was brought to your emergency department (ED) via ambulance.
Case Study One: Vital Signs. Susie is a nurse who works in a busy clinic in Philadelphia where a patient named Mr. Jones was added onto the schedule last minute because he is not feeling well. As ...
Let's consider a case study example: ... This chapter began with an introduction to the importance of measuring the vital signs in nursing practice. It went on to describe the measurement of each of the vital signs and the collection of other supporting data (e.g. height, weight, pain score), discussing key strategies and considerations. ...
Vital signs are an objective measurement of the essential physiological functions of a living organism. They have the name "vital" as their measurement and assessment is the critical first step for any clinical evaluation. The first set of clinical examinations is an evaluation of the vital signs of the patient. Triage of patients in an urgent/prompt care or an emergency department is based on ...
Monitoring vital signs for changes is important in nursing intervention to ensure safe patient care and improve patient outcomes. Vital signs include blood pressure, pulse rate, oxygen saturation ...
A series of high-level interactive clinical case studies is used to allow the audience to apply this new knowledge and practice methods of using vital signs to quickly narrow a diagnosis. Objectives Describe an algorithmic approach to assessing abnormal vital signs.
An electronic Case Report Form (eCRF) was used to collect study data. At each audit, documented vital sign data were collected: for vital signs fulfilling organisational pre‐MET and MET triggers (tailored to each organisation as per Table S1), data relating to any escalation of care per hospital policy were also collected. Data were collected ...
Case Study 4: Older Adult Client (continued) Vital Sign Measurements ... Print the blank vital sign record and document the adult client's vital sign readings. Then, go to the next page for a sample vital sign record of these findings. Vital Sign Record - Blank (pdf)
Vital signs' assessment is a key component of safe, high-quality care and a fundamental nursing priority. Trends in vital sign data provide early warning of impending sepsis and respiratory failure, and can independently predict mortality (Churpek et al, 2014; Nielsen et al, 2015).Furthermore, vital signs' data is important for medical emergency teams and early warning scores to function ...
Vital signs are typically obtained prior to performing a physical assessment. Vital signs include temperature recorded in Celsius or Fahrenheit, pulse, respiratory rate, blood pressure, and oxygen saturation using a pulse oximeter. See Figure 1.8 [1] for an image of a nurse obtaining vital signs. Obtaining vital signs may be delegated to ...
Case Study case studies, chapter 25, vital signs you are nurse caring for ironworker who has been admitted to your unit with acute hypertension. he became. Skip to document. University; High School. ... Nursing Fundamentals (Nurs 100) 999+ Documents. Students shared 1159 documents in this course. University West Coast University. Academic year ...
Critical-Thinking Questions about Case Studies; What Should the Nurse Do? Competency-Based Assessments; References; 5 Cultural Competence and Assessment. ... Even though it is not time to obtain the ordered vital signs, nursing judgment dictates the need to get another set of them. The vital signs are as follows: Temperature 99.8°F (37.7°C ...
Vital Signs Case Study. Mr. Sharma is a 73-year old gentleman who is hospitalized for pneumonia. He has history of heart failure and hypertension. He looks dyspneic and is mouth-breathing. Mr. Sharma also wears hearing aids. To establish a baseline assessment for Mr. Sharma, the nurse asks you to measure his vital signs.
Vital Sign Case Study 1. Which findings are considered abnormal for this adult client? What medical terminology is used to define/label these findings? - Client's blood pressure is above normal levels. Vital signs indicate that client has hypertension. 2. What factors might cause the blood pressure reading to be higher
Study with Quizlet and memorize flashcards containing terms like Mr. Charles Lamont is a 45-year-old patient who is visiting his primary care physician for his an annual checkup. His wife is waiting for him in the lobby; she is hoping that Mr. Lamont will tell the physician about his recent bout of coughing and shortness of breath. Mr. Lamont works for a construction company as a heavy machine ...
85 Case Study 1: Adult Client (continued) 1. What infection control measures should the healthcare provider implement? ... Orthostatic vital signs (pulse and blood pressure) should be taken because this client is at risk for hypovolemia. The client may be dehydrated as a result of the vomiting and diarrhea and lack of fluid intake. Return to ...
A Get the urinalysis (U/A) ordered by the doctor that needs to be sent to the lab. B Assess the lab results for the patient, focusing on the serum blood gas results. C Assess his Braden score because it due for the shift. D Assess his vital signs herself, verifying the UAP's findings. D Assess his vital signs herself, verifying the UAP's findings.
Nursing document from Cosumnes River College, 3 pages, Vital Sign Group Case Studies 1.) Mr. Coburn, a 56-year-old school teacher who was seen earlier in the week for hyperthermia, arrives at the walk-in health center complaining of feeling dizzy and nauseated. You immediately note that he appears to be havin
these demands is the case of pulseless electrical activity (PEA). In PEA, a patient's heart stops beating, causing un- ... Nursing is very protocol-driven so nurses are used to following checklist-like procedures. Also, nurses ... location of the vital signs monitor matter? A study of two trauma centers," 2010 American Medical Informatics As-
Future research is required to develop and evaluate a program that can achieve vital improvements in overall HRQOL, and potentially cardiovascular outcomes, of cardiac patients. We examined the effectiveness of depression treatment on healthrelated quality of life (HRQOL) of cardiac patients by conducting a meta-analysis using 5 randomized ...
On January 31, 2020, the Santa Clara County Department of Public Health (SCCDPH) in San Jose, California, USA, identified its first case of coronavirus disease (COVID-19) in a resident who had recently returned from Wuhan, China ().On February 28, the county reported its first case of COVID-19 associated with probable community transmission, 48 hours after the first presumed community-acquired ...
Sign/Symptom Symptom definition and additional criteria for when the child should stay home; Abdominal pain/stomachache Definition: Pain experienced anywhere between the chest and groin; pain may be continuous or may come and go. May attend school or child care unless the child has one of the following:. Pain is severe enough that child has difficulty participating in routine activities